
Contributions
Abstract: PB2351
Type: Publication Only
Background
Thrombotic microangiopathy (TMA) is a rare and life-threatening condition that can arise secondary to different diseases or mechanisms. The best known is the thrombotic thrombocytopenic purpura (TTP) a severe deficiency of ADAMTS13 in which an early treatment associates good prognosis, Hemolytic uremic syndrome (HUS) and Secondary TMA were the potential multiple etiologies can further delay diagnosis and treatment. The early detection of TMA can be done by both the clinical physician and hematology laboratory. In May of 2016 we started the implementation of the multidisciplinary team (MDT) in our center, in which the laboratory screens for early detection and works with the MDT when a TMA is suspected either by clinical or laboratory findings; decreasing the time for the diagnosis and treatment.
Aims
Retrospectively evaluate the improvement in the response time and detection of TMA cases with the joint effort of the MDT and the Hematology laboratory, in a single center.
Methods
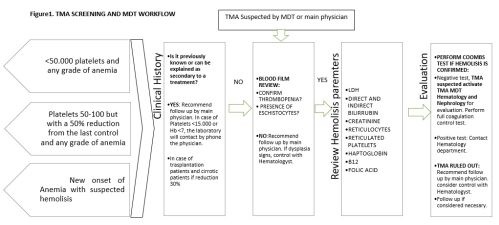
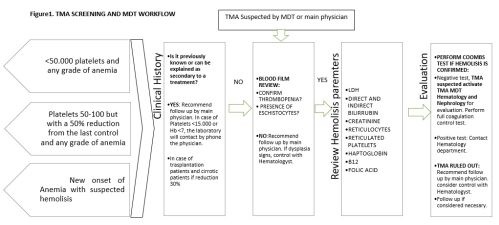
The MDT working group takes in physicians from Intensive care unit, Nephrology, Hematology, Farmacy, Immunology, and other services who follow the criteria for the diagnostic of TMA and discuss all potential TMA cases via a smartphone chat App, to elaborate the differential diagnoses and to recommend the best treatment option at every case. The screening evaluation is performed by a hematologist present in full time in the laboratory since 2015, either by critical results or a call from a suspected TMA case from the MDT. The laboratory screening and team workflow is described in figure 1. We report 44 cases from 2010-2017 (Including adults and children) with a median age 40-year-old. (1 – 76) from before and after the MDT group (table 1).
The Response time (RT) was retrospectively evaluated from the laboratory records, from the first day that a TMA diagnosis was feasible up to the day it was diagnosed.
Results
In the cohort of 44 cases there has been a dramatic increase in the detection of cases after the MDT group and screening was stablished, 2010 to Apr16 (15cases) versus >May16-Feb18 (29 cases) an increase of 65% of the diagnosis after the MDT. The median response time decreased from 11 days (1.5 – 12) before the MDT to 0 days (0-2) (P = 0.03) after the MDT. (table 1).
Table 1. Overall TMA diagnosis before and after MDT:
Cases
|
TMA |
Atypical HUS |
HUS |
TTP |
TMA transplant related |
Mean Response time |
2010– Apr 2016 |
15 | 10 | 0 | 2 | 3 | 11 days (1.5 – 12) |
May 2016 – Feb 2018 | 29 | 10 | 11 | 4 | 4 |
0 days (0-2) |
TOTAL | 44 | 20 | 11 | 6 | 7 | ---------------- |
Conclusion
The MDT communication with the laboratory and vice versa increases the awareness and detection of TMA, in which is fundamental to have a hematologist present in the laboratory and a trained staff to early recognize these alterations. The implementation of the MDT has improved the probability to early detect a TMA at our center. We believe that the Increase in the number of cases is probably related to missed or not diagnosed cases in the pre MDT era.
Session topic: 33. Platelets disorders
Keyword(s): Diagnosis, Thrombotic microangiopathy
Abstract: PB2351
Type: Publication Only
Background
Thrombotic microangiopathy (TMA) is a rare and life-threatening condition that can arise secondary to different diseases or mechanisms. The best known is the thrombotic thrombocytopenic purpura (TTP) a severe deficiency of ADAMTS13 in which an early treatment associates good prognosis, Hemolytic uremic syndrome (HUS) and Secondary TMA were the potential multiple etiologies can further delay diagnosis and treatment. The early detection of TMA can be done by both the clinical physician and hematology laboratory. In May of 2016 we started the implementation of the multidisciplinary team (MDT) in our center, in which the laboratory screens for early detection and works with the MDT when a TMA is suspected either by clinical or laboratory findings; decreasing the time for the diagnosis and treatment.
Aims
Retrospectively evaluate the improvement in the response time and detection of TMA cases with the joint effort of the MDT and the Hematology laboratory, in a single center.
Methods
The MDT working group takes in physicians from Intensive care unit, Nephrology, Hematology, Farmacy, Immunology, and other services who follow the criteria for the diagnostic of TMA and discuss all potential TMA cases via a smartphone chat App, to elaborate the differential diagnoses and to recommend the best treatment option at every case. The screening evaluation is performed by a hematologist present in full time in the laboratory since 2015, either by critical results or a call from a suspected TMA case from the MDT. The laboratory screening and team workflow is described in figure 1. We report 44 cases from 2010-2017 (Including adults and children) with a median age 40-year-old. (1 – 76) from before and after the MDT group (table 1).
The Response time (RT) was retrospectively evaluated from the laboratory records, from the first day that a TMA diagnosis was feasible up to the day it was diagnosed.
Results
In the cohort of 44 cases there has been a dramatic increase in the detection of cases after the MDT group and screening was stablished, 2010 to Apr16 (15cases) versus >May16-Feb18 (29 cases) an increase of 65% of the diagnosis after the MDT. The median response time decreased from 11 days (1.5 – 12) before the MDT to 0 days (0-2) (P = 0.03) after the MDT. (table 1).
Table 1. Overall TMA diagnosis before and after MDT:
Cases
|
TMA |
Atypical HUS |
HUS |
TTP |
TMA transplant related |
Mean Response time |
2010– Apr 2016 |
15 | 10 | 0 | 2 | 3 | 11 days (1.5 – 12) |
May 2016 – Feb 2018 | 29 | 10 | 11 | 4 | 4 |
0 days (0-2) |
TOTAL | 44 | 20 | 11 | 6 | 7 | ---------------- |
Conclusion
The MDT communication with the laboratory and vice versa increases the awareness and detection of TMA, in which is fundamental to have a hematologist present in the laboratory and a trained staff to early recognize these alterations. The implementation of the MDT has improved the probability to early detect a TMA at our center. We believe that the Increase in the number of cases is probably related to missed or not diagnosed cases in the pre MDT era.
Session topic: 33. Platelets disorders
Keyword(s): Diagnosis, Thrombotic microangiopathy


