
Contributions
Abstract: PB2065
Type: Publication Only
Background
Lymphomatoid granulomatosis is a rare, Epstein Barr Virus (EBV) associated systemic angiodestructive disorder which is considered a part of the spectrum of lymphoproliferative disorders. It usually presents in adulthood and uncommon in children. The incidence is higher in patients with immunodeficiency disorder. Pulmonary involvement occurs in over 90% cases and most of the time respiratory symptoms are initial sign of manifestation. The most common secondary HLH cause in pediatric population is EBV associated HLH.
Aims
Herein, we present a peripheral hemophagocytosis in a child with EBV associated lymphomatoid granulomatosis. Phagocytosis by peripheral blood monocytes occasionally be found on peripheral smears which may alert the physcian for evaluating bone marrow.
Methods
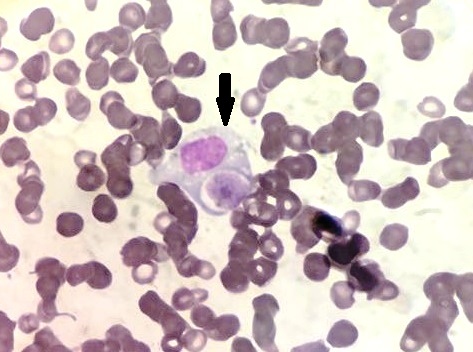
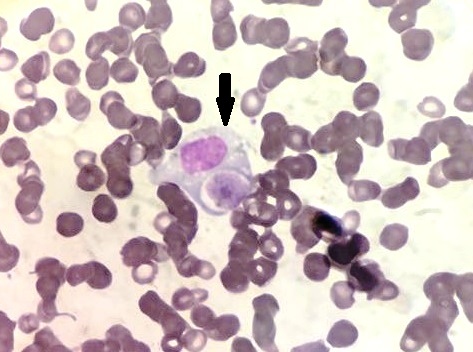
Case: A sixteen year-old female with an initial dignosis of sarcoidosis was admitted to the hospital with a complaints of cough, fever and fatigue. On her physical examination there were ecchymoses both at her arms and legs and pallor with hepatosplenomegaly. Laboratory evaluation revealed Hb:6,9g/dl, Hct:20,8%, platelet:64x109/L, WBC:0.9x109/L and examination of the peripheral blood by light microscopy revealed striking phagocytic activity by the monocytes with a differentiation of neutrophil %62, monocyte %12, lymphocyte %18, stab neutrophil %8 (figure 1). Her ferritin level was found to be increased at 963,6 ng/mL. Bone marrow examination showed prominent hemophagocytic histiocytes (HS), which is consistent with HLH. She received chemotherapy according to the HLH-2004 protocol, which includes etoposide, steroids, cyclosporin and ganciclovir as an antiviral treatment. In her follow up her pulmonary symptoms did not resolve and due to suspicions related to the previos diagnosis of sarcoidosis, a new Contrast Enhanced CT scan was done which showed pleural effusion at left hemithorax, bilateral mediastinal, paratracheal, subcarinal, hilar lymphadenopathy and boundless, centrilobular nodular opacities in both lungs. The EBV DNA in blood was 4208×103copy/mL. A previous lung biopsy was reevaluated and found that EBER was positive in granulamatous reaction which is compatible with lymphomatoid granulomatosis.
Results
The patient was treated with anti-CD20 immunotherapy (Rituximab, 375 mg/m2 intravenous infusion, four doses over a four week period). She got third doses of Rituximab, pulmonary lesions and HFS were resolved.
Conclusion
In our case EBV seems to be the responsible factor for both hemophagocytosis and lymphomatoid granulomatosis. Although the phagocytic activity of monocytes is well known it was occasionally find in the peripheral blood smear, in this case the interesting fact is that phagocytic activity is observed in the peripheral smear and bone marrow examination.
Session topic: 31. Infectious diseases, supportive care
Keyword(s): Children, EBV, Lymphoproliferative disorder
Abstract: PB2065
Type: Publication Only
Background
Lymphomatoid granulomatosis is a rare, Epstein Barr Virus (EBV) associated systemic angiodestructive disorder which is considered a part of the spectrum of lymphoproliferative disorders. It usually presents in adulthood and uncommon in children. The incidence is higher in patients with immunodeficiency disorder. Pulmonary involvement occurs in over 90% cases and most of the time respiratory symptoms are initial sign of manifestation. The most common secondary HLH cause in pediatric population is EBV associated HLH.
Aims
Herein, we present a peripheral hemophagocytosis in a child with EBV associated lymphomatoid granulomatosis. Phagocytosis by peripheral blood monocytes occasionally be found on peripheral smears which may alert the physcian for evaluating bone marrow.
Methods
Case: A sixteen year-old female with an initial dignosis of sarcoidosis was admitted to the hospital with a complaints of cough, fever and fatigue. On her physical examination there were ecchymoses both at her arms and legs and pallor with hepatosplenomegaly. Laboratory evaluation revealed Hb:6,9g/dl, Hct:20,8%, platelet:64x109/L, WBC:0.9x109/L and examination of the peripheral blood by light microscopy revealed striking phagocytic activity by the monocytes with a differentiation of neutrophil %62, monocyte %12, lymphocyte %18, stab neutrophil %8 (figure 1). Her ferritin level was found to be increased at 963,6 ng/mL. Bone marrow examination showed prominent hemophagocytic histiocytes (HS), which is consistent with HLH. She received chemotherapy according to the HLH-2004 protocol, which includes etoposide, steroids, cyclosporin and ganciclovir as an antiviral treatment. In her follow up her pulmonary symptoms did not resolve and due to suspicions related to the previos diagnosis of sarcoidosis, a new Contrast Enhanced CT scan was done which showed pleural effusion at left hemithorax, bilateral mediastinal, paratracheal, subcarinal, hilar lymphadenopathy and boundless, centrilobular nodular opacities in both lungs. The EBV DNA in blood was 4208×103copy/mL. A previous lung biopsy was reevaluated and found that EBER was positive in granulamatous reaction which is compatible with lymphomatoid granulomatosis.
Results
The patient was treated with anti-CD20 immunotherapy (Rituximab, 375 mg/m2 intravenous infusion, four doses over a four week period). She got third doses of Rituximab, pulmonary lesions and HFS were resolved.
Conclusion
In our case EBV seems to be the responsible factor for both hemophagocytosis and lymphomatoid granulomatosis. Although the phagocytic activity of monocytes is well known it was occasionally find in the peripheral blood smear, in this case the interesting fact is that phagocytic activity is observed in the peripheral smear and bone marrow examination.
Session topic: 31. Infectious diseases, supportive care
Keyword(s): Children, EBV, Lymphoproliferative disorder


