
Contributions
Abstract: PB2205
Type: Publication Only
Background
Solitary plasmacytomas of the bone (SPB) are malignant, intramedullary, monoclonal plasma cell expansions in absence of systemic myelomatous disease. Left untreated, many SPB progress to systemic multiple myeloma (MM). Adequate and timely treatment is vital, since SPB represent a window of curative opportunity that is lost with progression to MM. The current gold standard for SPB treatment is radiotherapy (RT). However, a recent population study (Thumallapally et a, 2017), suggested that additional surgical treatment improves patient survival.
Aims
We reviewed the literature and performed a meta-analysis to assess the use and effect of surgery in SPB.
Methods
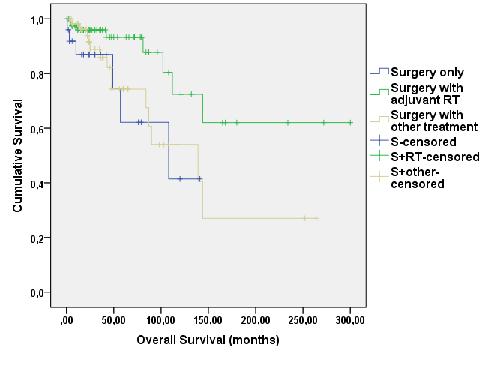
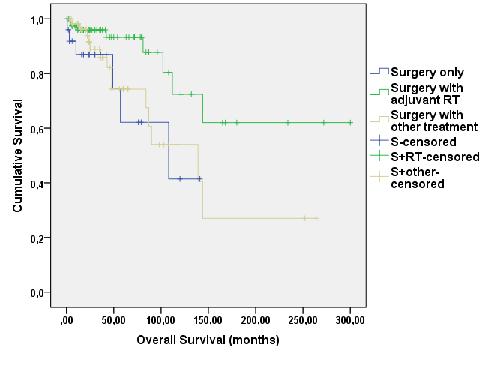
We searched PubMed, EMBASE and Web of Science for papers describing cases of surgically treated SPB. We included original reports from clinical practise written in Dutch or English from 1990 or later describing ≥1 case of surgically treated SPB without evidence of systemic myelomatous disease at the time of diagnosis. Individually described cases for which intervention and follow-up data were available, were analysed in Kaplan-Meier plots.
Results
From 709 results, we included 113 suitable papers describing 700 SPB cases in total (skull and facial bones: 98; spine: 300; chest wall: 98; pelvis: 69; extremities: 86; unspecified: 49). Intriguingly, only 4 authors stated that their surgical intervention was driven by consideration for the patient’s prognosis. More commonly, surgical intervention was performed due to initial misdiagnosis of the lesion or the need for acute intervention. In the skull, many authors performed craniotomies expecting to find meningiomas, spinal SPB was mostly operated upon for decompression and stabilisation and SPB of the extremities often presented as a pathological fracture with a need for stabilisation with osteosynthetic material. 195 cases were described in adequate detail to be included in a survival analysis. The male to female ratio was 2,2:1 and median age at diagnosis 53 years (range: 5-82), in line with previously published population data. Skull SPB cases were disproportionally often female (p=0,016). No other sex or age preference was observed between SPB localisations. Kaplan-Meier survival analysis showed better overall survival for combined treatment with surgery and RT (n=79) over surgery alone (n=25)(p=0,020) or surgery in combination with other treatment (n=53)(p=0,021). Progression-free survival was not significantly different between treatments. Our cohort had too few cases treated by RT alone to yield significant results.
Conclusion
Although surgical intervention with adjuvant RT was shown to confer the best survival in population studies, the choice for surgical intervention is rarely made for the benefit of long-term patient survival. Our findings warrant consideration of additional surgical excision to the treatment plan of patients otherwise treated by RT alone. Moreover, SPB patients who undergo surgical intervention for stabilisation, central nervous system decompression, diagnostic excision etc., may clearly benefit from adjuvant RT. Comprising only case reports, case series and retrospective cohorts, the papers included in this study are at a high risk for selection bias. Therefore we recommend validating these results in a prospective clinical trial. Additionally, these outcomes may be compared with patients treated by RT alone, and the research question may be extended to solitary extramedullary plasmacytomas and plasmacytomas in the context of MM.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Plasma cells, Radiotherapy, Surgery, Survival
Abstract: PB2205
Type: Publication Only
Background
Solitary plasmacytomas of the bone (SPB) are malignant, intramedullary, monoclonal plasma cell expansions in absence of systemic myelomatous disease. Left untreated, many SPB progress to systemic multiple myeloma (MM). Adequate and timely treatment is vital, since SPB represent a window of curative opportunity that is lost with progression to MM. The current gold standard for SPB treatment is radiotherapy (RT). However, a recent population study (Thumallapally et a, 2017), suggested that additional surgical treatment improves patient survival.
Aims
We reviewed the literature and performed a meta-analysis to assess the use and effect of surgery in SPB.
Methods
We searched PubMed, EMBASE and Web of Science for papers describing cases of surgically treated SPB. We included original reports from clinical practise written in Dutch or English from 1990 or later describing ≥1 case of surgically treated SPB without evidence of systemic myelomatous disease at the time of diagnosis. Individually described cases for which intervention and follow-up data were available, were analysed in Kaplan-Meier plots.
Results
From 709 results, we included 113 suitable papers describing 700 SPB cases in total (skull and facial bones: 98; spine: 300; chest wall: 98; pelvis: 69; extremities: 86; unspecified: 49). Intriguingly, only 4 authors stated that their surgical intervention was driven by consideration for the patient’s prognosis. More commonly, surgical intervention was performed due to initial misdiagnosis of the lesion or the need for acute intervention. In the skull, many authors performed craniotomies expecting to find meningiomas, spinal SPB was mostly operated upon for decompression and stabilisation and SPB of the extremities often presented as a pathological fracture with a need for stabilisation with osteosynthetic material. 195 cases were described in adequate detail to be included in a survival analysis. The male to female ratio was 2,2:1 and median age at diagnosis 53 years (range: 5-82), in line with previously published population data. Skull SPB cases were disproportionally often female (p=0,016). No other sex or age preference was observed between SPB localisations. Kaplan-Meier survival analysis showed better overall survival for combined treatment with surgery and RT (n=79) over surgery alone (n=25)(p=0,020) or surgery in combination with other treatment (n=53)(p=0,021). Progression-free survival was not significantly different between treatments. Our cohort had too few cases treated by RT alone to yield significant results.
Conclusion
Although surgical intervention with adjuvant RT was shown to confer the best survival in population studies, the choice for surgical intervention is rarely made for the benefit of long-term patient survival. Our findings warrant consideration of additional surgical excision to the treatment plan of patients otherwise treated by RT alone. Moreover, SPB patients who undergo surgical intervention for stabilisation, central nervous system decompression, diagnostic excision etc., may clearly benefit from adjuvant RT. Comprising only case reports, case series and retrospective cohorts, the papers included in this study are at a high risk for selection bias. Therefore we recommend validating these results in a prospective clinical trial. Additionally, these outcomes may be compared with patients treated by RT alone, and the research question may be extended to solitary extramedullary plasmacytomas and plasmacytomas in the context of MM.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Plasma cells, Radiotherapy, Surgery, Survival


