
Contributions
Abstract: PB1933
Type: Publication Only
Background
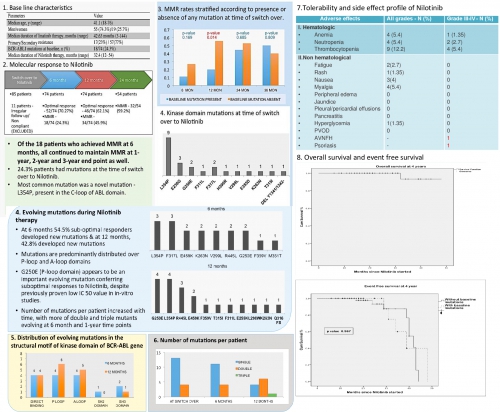
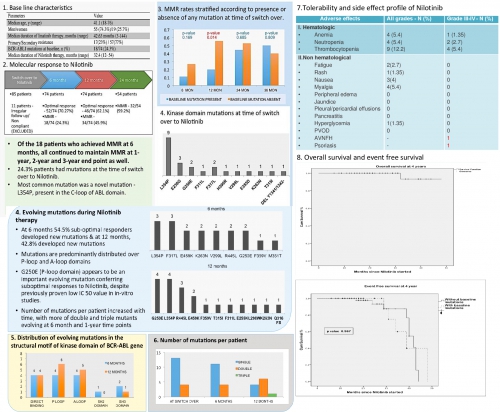
Nilotinib is a second generation tyrosine kinase inhibitor (TKI) approved for adults with newly diagnosed chronic myeloid leukemia (CML) in chronic phase (CP) and those with Imatinib-resistant or intolerant CML-CP and CML in accelerated phase (AP). The occurrence and impact of baseline as well as evolving kinase domain (KD) mutations on Nilotinib therapy were assessed in this study. Also, no Indian data is available till date on the efficacy of second line nilotinib and this study reflects a real world data from a developing country with resource-constrained setting
Aims
Primary objectives were to assess the molecular response as well as the prevalence, pattern and evolution of KD mutations before and during second line Nilotinib therapy in CML- CP patients.
Methods
Patients of CML-CP aged ≥ 18 years, who developed Imatinib-resistance or Imatinib-intolerance and thus switched to second line Nilotinib therapy, were included. KD mutation analysis was done retrospectively in the stored cDNA of samples extracted for BCR ABL analysis, by Sanger’s direct sequencing. Mutation analysis was repeated when there was a suboptimal response/loss of response at 6 months and 12-month time points.
Results
Of the total 674 newly diagnosed CML patients presented from January 2013 - June 2016, 85 (12.6%) patients were started on Nilotinib, of which 11 patients were non compliant/irregular in follow up and thus excluded from further analysis. 18 patients (24.3%) had BCR-ABL KD mutations at the time of switch over to Nilotinib. Median duration of Nilotinib therapy was 32.4 months, with a minimum follow up of at least 12 months. Optimal response was achieved in 70.27% patients at 6 months of Nilotinib therapy, of which major molecular response (MMR) rate was 24.3%. All 18 patients who achieved MMR at 6 months continued to maintain MMR till last follow up (median duration - 28.6 months). Of the suboptimal responders, 54.5% patients had evolution of new mutations at 6 months. At 1-year end point, 45.9% patients achieved MMR and 42.8% of the suboptimal responders had evolution of new mutations, especially in P-loop and A-loop domains. Number of mutations per patient increased with time, with more of double and triple mutants evolving at 6 month and 1-year time points. When stratified according to presence or absence of any mutations at switch over, significantly better MMR rates at 1 year were seen in mutation negative group (20% vs. 55.5%, p= 0.014). Estimated 4-year overall survival and EFS of the cohort was 93.3% and 38.6%. Only 4 (5.4%) patients developed Grade III-IV hematologic toxicity. 2 patients who developed blast crisis died.
Conclusion
Nilotinib is an effective second line TKI with 24.3%, 45.9% and 59.2% MMR rates at 6 months, 1 year and 2 year, respectively. Achievement of MMR at 6 months predicts long-term stable molecular remissions.So, earlier and deeper molecular kinetics can be used as a prognostic marker to identify low-risk patient subsets. Evolving new unfavourable mutations are major causes of treatment failure. In contrary to ELN guidelines, all new mutations need not necessarily imply to label a TKI failure and does not warrant a change in therapy, especially in a developing country like India. Side effects are usually well tolerated, most common being cytopenias. Large-scale studies with long-term follow up are required for assessing the durability of sustained MMR with Nilotinib and to broaden the spectrum of clinically significant mutations influencing the TKI therapy.
Session topic: 8. Chronic myeloid leukemia - Clinical
Keyword(s): Chronic myeloid leukemia, Kinase domain mutant, Molecular response, Tyrosine kinase inhibitor
Abstract: PB1933
Type: Publication Only
Background
Nilotinib is a second generation tyrosine kinase inhibitor (TKI) approved for adults with newly diagnosed chronic myeloid leukemia (CML) in chronic phase (CP) and those with Imatinib-resistant or intolerant CML-CP and CML in accelerated phase (AP). The occurrence and impact of baseline as well as evolving kinase domain (KD) mutations on Nilotinib therapy were assessed in this study. Also, no Indian data is available till date on the efficacy of second line nilotinib and this study reflects a real world data from a developing country with resource-constrained setting
Aims
Primary objectives were to assess the molecular response as well as the prevalence, pattern and evolution of KD mutations before and during second line Nilotinib therapy in CML- CP patients.
Methods
Patients of CML-CP aged ≥ 18 years, who developed Imatinib-resistance or Imatinib-intolerance and thus switched to second line Nilotinib therapy, were included. KD mutation analysis was done retrospectively in the stored cDNA of samples extracted for BCR ABL analysis, by Sanger’s direct sequencing. Mutation analysis was repeated when there was a suboptimal response/loss of response at 6 months and 12-month time points.
Results
Of the total 674 newly diagnosed CML patients presented from January 2013 - June 2016, 85 (12.6%) patients were started on Nilotinib, of which 11 patients were non compliant/irregular in follow up and thus excluded from further analysis. 18 patients (24.3%) had BCR-ABL KD mutations at the time of switch over to Nilotinib. Median duration of Nilotinib therapy was 32.4 months, with a minimum follow up of at least 12 months. Optimal response was achieved in 70.27% patients at 6 months of Nilotinib therapy, of which major molecular response (MMR) rate was 24.3%. All 18 patients who achieved MMR at 6 months continued to maintain MMR till last follow up (median duration - 28.6 months). Of the suboptimal responders, 54.5% patients had evolution of new mutations at 6 months. At 1-year end point, 45.9% patients achieved MMR and 42.8% of the suboptimal responders had evolution of new mutations, especially in P-loop and A-loop domains. Number of mutations per patient increased with time, with more of double and triple mutants evolving at 6 month and 1-year time points. When stratified according to presence or absence of any mutations at switch over, significantly better MMR rates at 1 year were seen in mutation negative group (20% vs. 55.5%, p= 0.014). Estimated 4-year overall survival and EFS of the cohort was 93.3% and 38.6%. Only 4 (5.4%) patients developed Grade III-IV hematologic toxicity. 2 patients who developed blast crisis died.
Conclusion
Nilotinib is an effective second line TKI with 24.3%, 45.9% and 59.2% MMR rates at 6 months, 1 year and 2 year, respectively. Achievement of MMR at 6 months predicts long-term stable molecular remissions.So, earlier and deeper molecular kinetics can be used as a prognostic marker to identify low-risk patient subsets. Evolving new unfavourable mutations are major causes of treatment failure. In contrary to ELN guidelines, all new mutations need not necessarily imply to label a TKI failure and does not warrant a change in therapy, especially in a developing country like India. Side effects are usually well tolerated, most common being cytopenias. Large-scale studies with long-term follow up are required for assessing the durability of sustained MMR with Nilotinib and to broaden the spectrum of clinically significant mutations influencing the TKI therapy.
Session topic: 8. Chronic myeloid leukemia - Clinical
Keyword(s): Chronic myeloid leukemia, Kinase domain mutant, Molecular response, Tyrosine kinase inhibitor


