
Contributions
Abstract: PB1928
Type: Publication Only
Background
The results of long-term follow-up of patients with chronic myelogenous leukemia (CML) do not lose their importance. The use of TKI (imatinib, IM) resulted to dramatic improvement in survival, so probability of CML-related death for patients (pts) could be significantly lower than chance of dying due to common mortality causes besides than CML.
Aims
To analyze overall survival (OS) and causes of mortality in CML pts treated in routine clinical practice in Russian Federation for a long period (>12 years) of time.
Methods
The analyzed cohort consisted of 607 Ph/BCR-ABL-positive CML pts from 29 regions of Russia (ELN OSP EUTOS) diagnosed in 2002- 2006 with IM therapy initiation ≤6 months (mo) after diagnosis established. Median (Me) of age was 48(18-82) years (y), 47% males. Pretreatment regimens were as follows: hydroxyurea 454(76%) pts; chemotherapy 25(4%) pts, IFN-α 37(6%) pts. Chronic phase (CP) of CML was diagnosed in 557 (93%) pts, accelerated phase (AP) - 38(6%) and blast crisis (BC) – in 6(1%) pts. The number of patients with CML according to years of diagnosis were: 2002 - 15pts, 2003 - 38pts, 2004 - 46pts, 2005 - 206pts, 2006 - 302pts. Last database update had been made on Nov. 2017 for 473 pts; in addition, 134 pts from 2 regions were updated in 2015.
Results
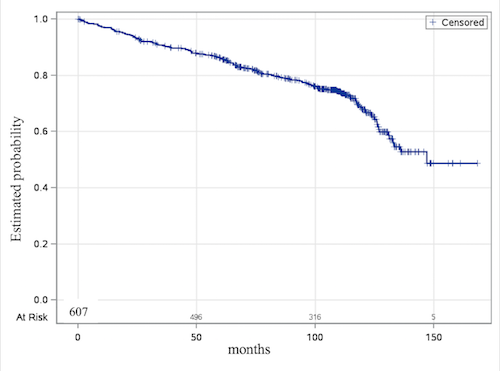
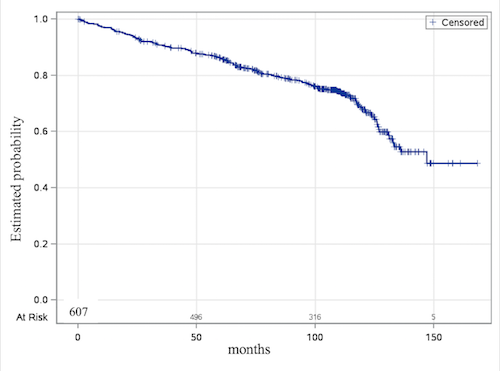
The median follow-up was 92,4 (1- 170,3) mo. At 12 years, OS was 50%(figure 1); OS by age groups were: 20-40yy- 68%, 40-60yy- 69%, 60-80yy- 40%. Mortality in the whole cohort of 607 pts was 27% (168 pts). Of these 168 pts, 91(54,2%)pts deaths were as results of CML progression to AP or BP including non-complaent cases; 3pts (1,7%) were reported as died in CP CML, 3pts (1,7%) - after allogeneic stem cell transplantation (2 due to infection complications), in 19 (11,4%) cause of death was unknown. Deaths caused by concomitant diseases were in 52 cases (31%): coronary artery disease/myocardial infarction/heart failure in 18 cases, acute ischemic stroke in 8 cases, second malignancies (Cr) in 8 cases (lung tumor, metastatic esophageal Cr, stomach Cr, brain tumor, Cr of the sigmoid colon, Cr of rectal and colon, melanoma, renal Cr), accidents - 2 cases, liver cirrhosis in 2 pts, in 2 cases – respiratory virus infections complicated with pneumonia and others.
Conclusion
Long-term follow-up of patients participated in the tracked cohort of 607 patients in the OSP EUTOS study allowed to characterize the results of OS and the cause of death according to age and comorbidity. The cause of death in our study in 34% of cases was unrelated to CML, which corresponds to the reference data (Castagnetti 2013, Hehlmann 2014, Pfirrmann 2015). Mortalities related to cardiovascular causes and second malignancies in pts with CML have significant proportion (50% and 15% from the whole mortality, respectively). A substantial reduction of OS from 78 to 50% is observed after 8 to 12 years of TKI therapy due to cohort aging and dying out for ordinary reasons.
Session topic: 8. Chronic myeloid leukemia - Clinical
Keyword(s): Survival, Chronic myeloid leukemia, Comorbidities, Long-term follow-up
Abstract: PB1928
Type: Publication Only
Background
The results of long-term follow-up of patients with chronic myelogenous leukemia (CML) do not lose their importance. The use of TKI (imatinib, IM) resulted to dramatic improvement in survival, so probability of CML-related death for patients (pts) could be significantly lower than chance of dying due to common mortality causes besides than CML.
Aims
To analyze overall survival (OS) and causes of mortality in CML pts treated in routine clinical practice in Russian Federation for a long period (>12 years) of time.
Methods
The analyzed cohort consisted of 607 Ph/BCR-ABL-positive CML pts from 29 regions of Russia (ELN OSP EUTOS) diagnosed in 2002- 2006 with IM therapy initiation ≤6 months (mo) after diagnosis established. Median (Me) of age was 48(18-82) years (y), 47% males. Pretreatment regimens were as follows: hydroxyurea 454(76%) pts; chemotherapy 25(4%) pts, IFN-α 37(6%) pts. Chronic phase (CP) of CML was diagnosed in 557 (93%) pts, accelerated phase (AP) - 38(6%) and blast crisis (BC) – in 6(1%) pts. The number of patients with CML according to years of diagnosis were: 2002 - 15pts, 2003 - 38pts, 2004 - 46pts, 2005 - 206pts, 2006 - 302pts. Last database update had been made on Nov. 2017 for 473 pts; in addition, 134 pts from 2 regions were updated in 2015.
Results
The median follow-up was 92,4 (1- 170,3) mo. At 12 years, OS was 50%(figure 1); OS by age groups were: 20-40yy- 68%, 40-60yy- 69%, 60-80yy- 40%. Mortality in the whole cohort of 607 pts was 27% (168 pts). Of these 168 pts, 91(54,2%)pts deaths were as results of CML progression to AP or BP including non-complaent cases; 3pts (1,7%) were reported as died in CP CML, 3pts (1,7%) - after allogeneic stem cell transplantation (2 due to infection complications), in 19 (11,4%) cause of death was unknown. Deaths caused by concomitant diseases were in 52 cases (31%): coronary artery disease/myocardial infarction/heart failure in 18 cases, acute ischemic stroke in 8 cases, second malignancies (Cr) in 8 cases (lung tumor, metastatic esophageal Cr, stomach Cr, brain tumor, Cr of the sigmoid colon, Cr of rectal and colon, melanoma, renal Cr), accidents - 2 cases, liver cirrhosis in 2 pts, in 2 cases – respiratory virus infections complicated with pneumonia and others.
Conclusion
Long-term follow-up of patients participated in the tracked cohort of 607 patients in the OSP EUTOS study allowed to characterize the results of OS and the cause of death according to age and comorbidity. The cause of death in our study in 34% of cases was unrelated to CML, which corresponds to the reference data (Castagnetti 2013, Hehlmann 2014, Pfirrmann 2015). Mortalities related to cardiovascular causes and second malignancies in pts with CML have significant proportion (50% and 15% from the whole mortality, respectively). A substantial reduction of OS from 78 to 50% is observed after 8 to 12 years of TKI therapy due to cohort aging and dying out for ordinary reasons.
Session topic: 8. Chronic myeloid leukemia - Clinical
Keyword(s): Survival, Chronic myeloid leukemia, Comorbidities, Long-term follow-up


