
Contributions
Abstract: PB1878
Type: Publication Only
Background
In addition to blocking signals of cell proliferation, BCR tyrosine kinases inhibitors (BCR inhibitors) also inhibit other signalling pathways, such as toll-like receptors, which are essential for the control of infections. There are few real-life data on the infectious risk associated to ibrutinib and idelalisib.
Aims
To analyse the incidence of the infections in patients receiving treatment with BCR inhibitors and to identify predisposing factors for the development of infections in these patients.
Methods
Data were collected retrospectively, including patients diagnosed with chronic lymphocytic leukemia (CLL) who have received BCR inhibitors for more than 1 month, in Virgen de las Nieves University Hospital in Granada (Spain), from June 2015 to February 2018. Patients received ibrutinib in monotherapy and/or idelalisib-rituximab, and prophylaxis with aciclovir and trimethoprim/sulphamethoxazole.
Results
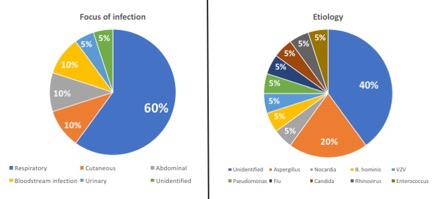
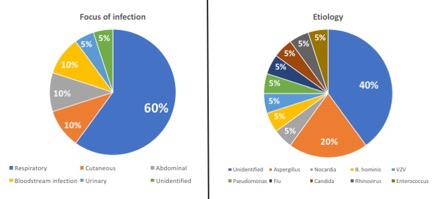
22 patients were treated with BCR inhibitors: 11 with ibrutinib, 6 with idelalisib-rituximab and 5 with both treatments, sequentially. Patient characteristics are shown in Table 1. During the follow-up period, 33 episodes of infections occurred, with 20 of them (60.6%) requiring hospital admission and occurring in 11 patients. The focus and etiology are shown in Graph 1. The mean number of days of treatment prior to the first episode of infection (grade ≥3) was 101 days, 54.5% and 27.3% of them after 3 and 6 months, respectively. We observed a positive correlation between the probability of infection (grade ≥3) and the CIRS score (p<0.05), and also an almost statistically significant and positive correlation between the probability of infection and the number of previous treatment lines (p=0.051). Age, cytogenetic status, type of BCR inhibitor and the diagnosis-to-treatment time, have were not predictive factors of hospital admission. Pulmonary aspergillosis was diagnosed in 4 patients (18.2%), with a trend for a correlation between the risk for this fungal infection and the CIRS score (p=0.08) and the number of previous treatment lines (p=0.054). Finally, infection-related global mortality was 27.3% (6 patients) due to pulmonary aspergillosis (2 patients), bloodstream infection by Enterococcus faecium (1 patient), varicella-zoster virus (1 patient), flu (1 patient) and respiratory infection without clear etiology (1 patient). The average number of days from the start of treatment to death was 298 days.
Table 1: Clinical characteristics of the patients (average) | |||
Male 54.5% | Age 67 years | CIRS score 8.3 | CIRS score 8.3 |
Treatment with ibrutinib and idelalisib-rituximab 72.7% and 50% | Nº of previous treatment lines 2.1 | 17p-/TP53 mutated 54.5% | |
Conclusion
Infectious complications were greater than expected, being the main cause of discontinuation. Furthermore, they required hospital admission in more than half of the cases with a considerable mortality. CIRS score and the number of previous treatment lines were predictors of serious infections. Therefore, it seems advisable for patients with multiple treatments and comorbidities not to delay the treatment with BCR inhibitors to avoid infectious complications that may cause treatment discontinuation. With the high incidence of pulmonary aspergillosis in our series, specific strategies for the early detection, treatment and prophylaxis should be adopted. More studies in real-life settings are needed.
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): Chronic Lymphocytic Leukemia, Comorbidities, Infection, Risk factor
Abstract: PB1878
Type: Publication Only
Background
In addition to blocking signals of cell proliferation, BCR tyrosine kinases inhibitors (BCR inhibitors) also inhibit other signalling pathways, such as toll-like receptors, which are essential for the control of infections. There are few real-life data on the infectious risk associated to ibrutinib and idelalisib.
Aims
To analyse the incidence of the infections in patients receiving treatment with BCR inhibitors and to identify predisposing factors for the development of infections in these patients.
Methods
Data were collected retrospectively, including patients diagnosed with chronic lymphocytic leukemia (CLL) who have received BCR inhibitors for more than 1 month, in Virgen de las Nieves University Hospital in Granada (Spain), from June 2015 to February 2018. Patients received ibrutinib in monotherapy and/or idelalisib-rituximab, and prophylaxis with aciclovir and trimethoprim/sulphamethoxazole.
Results
22 patients were treated with BCR inhibitors: 11 with ibrutinib, 6 with idelalisib-rituximab and 5 with both treatments, sequentially. Patient characteristics are shown in Table 1. During the follow-up period, 33 episodes of infections occurred, with 20 of them (60.6%) requiring hospital admission and occurring in 11 patients. The focus and etiology are shown in Graph 1. The mean number of days of treatment prior to the first episode of infection (grade ≥3) was 101 days, 54.5% and 27.3% of them after 3 and 6 months, respectively. We observed a positive correlation between the probability of infection (grade ≥3) and the CIRS score (p<0.05), and also an almost statistically significant and positive correlation between the probability of infection and the number of previous treatment lines (p=0.051). Age, cytogenetic status, type of BCR inhibitor and the diagnosis-to-treatment time, have were not predictive factors of hospital admission. Pulmonary aspergillosis was diagnosed in 4 patients (18.2%), with a trend for a correlation between the risk for this fungal infection and the CIRS score (p=0.08) and the number of previous treatment lines (p=0.054). Finally, infection-related global mortality was 27.3% (6 patients) due to pulmonary aspergillosis (2 patients), bloodstream infection by Enterococcus faecium (1 patient), varicella-zoster virus (1 patient), flu (1 patient) and respiratory infection without clear etiology (1 patient). The average number of days from the start of treatment to death was 298 days.
Table 1: Clinical characteristics of the patients (average) | |||
Male 54.5% | Age 67 years | CIRS score 8.3 | CIRS score 8.3 |
Treatment with ibrutinib and idelalisib-rituximab 72.7% and 50% | Nº of previous treatment lines 2.1 | 17p-/TP53 mutated 54.5% | |
Conclusion
Infectious complications were greater than expected, being the main cause of discontinuation. Furthermore, they required hospital admission in more than half of the cases with a considerable mortality. CIRS score and the number of previous treatment lines were predictors of serious infections. Therefore, it seems advisable for patients with multiple treatments and comorbidities not to delay the treatment with BCR inhibitors to avoid infectious complications that may cause treatment discontinuation. With the high incidence of pulmonary aspergillosis in our series, specific strategies for the early detection, treatment and prophylaxis should be adopted. More studies in real-life settings are needed.
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): Chronic Lymphocytic Leukemia, Comorbidities, Infection, Risk factor


