
Contributions
Abstract: PB2053
Type: Publication Only
Background
It is known that patients undergoing intensive induction chemotherapy (IIC) for acute myeloid leukemia (AML) have a high risk for developing infectious complications.
Aims
To describe microbiologically documented infectious episodes, the use of antimicrobials and the outcome of all consecutive patients undergoing IIC for newly diagnosed AML during the last 4 years.
Methods
A total of 111 adult patients were diagnosed with AML at the Donostia University Hospital from 2014 to 2017. Patients with AML-M3 (8 pts) and those who did not receive IIC (48 pts) were excluded for this analysis. In total, 55 pts were treated with IIC: 50 with Ida + Ara-C (3 + 7) and 5 with Flag-Ida. The median age was 61 years (23-78). 30 were men and 25 women. Most of the pts (88%) stayed in HEPA-filtered rooms.
Results
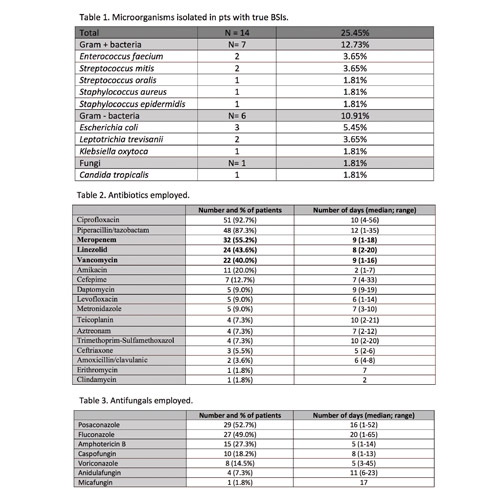
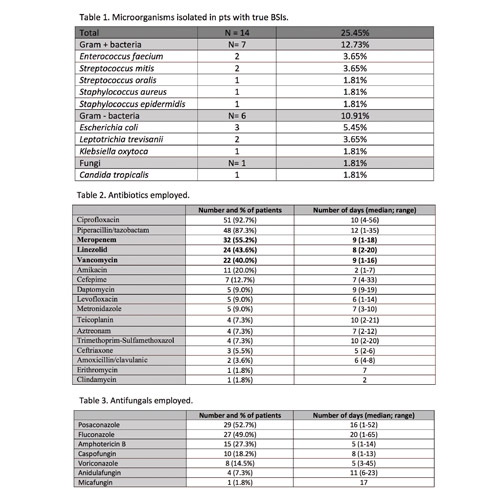
Median hospital admission was 30 days (22-77). Five pts (9.1%) died during admission. Thirty one pts (56.4%) achieved complete remission after the IIC. A total of 336 blood cultures (BC) were performed (average: 6.11 BC/pt, range: 1-17). 21 BC (6.25%) were positive (false positives were excluded). Fourteen pts (25.45%) had at least 1 true bloodstream infection (BSI), whose characteristics are shown in Table 1. Other cultures performed were: urine (136), stool (98) and others (38). The antimicrobials used are shown in Tables 2 and 3. Only one of the 5 pts who died was due to infectious mortality (1.81%) (sepsis due to Candida tropicalis). No other IFI cases were documented.
Conclusion
1) fungal BSIs, in general, and IFI incidence, in particular, were very low in this group of high risk pts (1.81%). This fact could be attributed to the combination of several factors: a) the majority of the pts stayed in HEPA-filtered rooms; b) the antifungal prophylaxis used; c) the use of empirical antifungal therapy for prolonged neutropenic fever. 2) Bacterial BSIs were relatively frequent (23.64%) among patients undergoing IIC for newly diagnosed AML. Gram + bacteria (12.73%) were slightly predominant over Gram - bacteria (10.91%). There was no mortality due to a bacterial infection. Our analysis shows, however, a high consumption of carbapenems (55.2% of pts), vancomycin (43.6% of pts) and linezolid (22% of pts). Due to the growing concern and awareness of the problems of antibiotic resistance around the world, we recently implemented a new protocol for the management of fever, more conservative and restrictive, with the hope of reducing the use of unnecessary antibiotics, maintaining the low rate of infectious mortality.
Session topic: 31. Infectious diseases, supportive care
Keyword(s): AML, Infection
Abstract: PB2053
Type: Publication Only
Background
It is known that patients undergoing intensive induction chemotherapy (IIC) for acute myeloid leukemia (AML) have a high risk for developing infectious complications.
Aims
To describe microbiologically documented infectious episodes, the use of antimicrobials and the outcome of all consecutive patients undergoing IIC for newly diagnosed AML during the last 4 years.
Methods
A total of 111 adult patients were diagnosed with AML at the Donostia University Hospital from 2014 to 2017. Patients with AML-M3 (8 pts) and those who did not receive IIC (48 pts) were excluded for this analysis. In total, 55 pts were treated with IIC: 50 with Ida + Ara-C (3 + 7) and 5 with Flag-Ida. The median age was 61 years (23-78). 30 were men and 25 women. Most of the pts (88%) stayed in HEPA-filtered rooms.
Results
Median hospital admission was 30 days (22-77). Five pts (9.1%) died during admission. Thirty one pts (56.4%) achieved complete remission after the IIC. A total of 336 blood cultures (BC) were performed (average: 6.11 BC/pt, range: 1-17). 21 BC (6.25%) were positive (false positives were excluded). Fourteen pts (25.45%) had at least 1 true bloodstream infection (BSI), whose characteristics are shown in Table 1. Other cultures performed were: urine (136), stool (98) and others (38). The antimicrobials used are shown in Tables 2 and 3. Only one of the 5 pts who died was due to infectious mortality (1.81%) (sepsis due to Candida tropicalis). No other IFI cases were documented.
Conclusion
1) fungal BSIs, in general, and IFI incidence, in particular, were very low in this group of high risk pts (1.81%). This fact could be attributed to the combination of several factors: a) the majority of the pts stayed in HEPA-filtered rooms; b) the antifungal prophylaxis used; c) the use of empirical antifungal therapy for prolonged neutropenic fever. 2) Bacterial BSIs were relatively frequent (23.64%) among patients undergoing IIC for newly diagnosed AML. Gram + bacteria (12.73%) were slightly predominant over Gram - bacteria (10.91%). There was no mortality due to a bacterial infection. Our analysis shows, however, a high consumption of carbapenems (55.2% of pts), vancomycin (43.6% of pts) and linezolid (22% of pts). Due to the growing concern and awareness of the problems of antibiotic resistance around the world, we recently implemented a new protocol for the management of fever, more conservative and restrictive, with the hope of reducing the use of unnecessary antibiotics, maintaining the low rate of infectious mortality.
Session topic: 31. Infectious diseases, supportive care
Keyword(s): AML, Infection


