
Contributions
Abstract: PB2457
Type: Publication Only
Background
The allogenic stem cell transplantation (Allo-HSCT) is an efficient treatment for patients with high risk hematologic malignancies. Over the past decades new modalities of Allo-HSCT as Haploidentical stem cell transplantation (Haplo-HSCT) allowed us to offer this therapy to patients who for race reasons, presence of rare haplotypes or rapidly progressive disease course can’t find a compatible unrelated donor.
Aims
The aim of this study is to assess the efficacy of Haplo-HSCT on our series evaluating the survival (S), overall mortality (OM) at 100 days and transplant related mortality (TRM).
Methods
We analyzed all the consecutive Haplo-HSCT performed in our center since 2013. The conditioning regimens were decided regarding age, comorbidities and pre-Haplo-HSCT disease status. All patients received high doses of Cy (50 mg/kg on days 3 and 4 posttransplantation) cyclosporine and MMF as CGvHD prophylaxis. We classified the patients before the Haplo-HSCT according to performance status (ECOG), comorbidities (Sorror), disease status (DRI and EBMT). We used SPSS V.23 to calculate the S and OM by the KM test and Chi squared tests.
Results
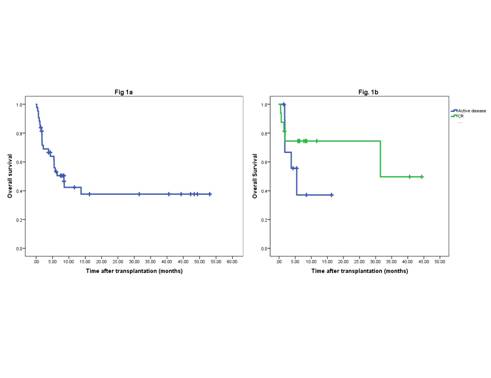
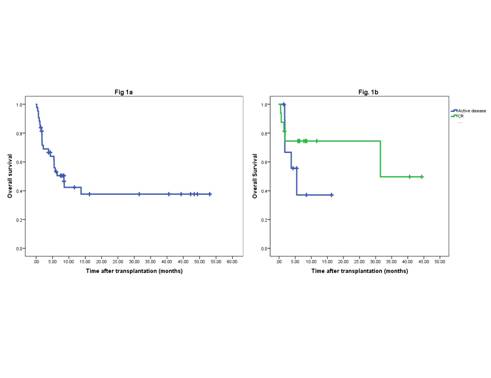
We performed 43 haplo-HSCT, 25 were males and 18 females with a mean age of 43 (range 16- 68). Diagnosis: Acute myeloid leukemia (24), Acute lymphoid leukemia (3), Hodgkin disease (65), Non Hodgkin lymphoma (2), severe aplastic anemia (2) Chronic lymphoproliferative disease (3). 23/43 patients died throughout the follow-up period with 31% OM at day +100 (fig. 1a). 15/23 patients died due to TRM. 7/8 of the remaining patients died due to disease progression and 5 out of these 7 patients had an active disease pre-Haplo-HSCT. For the analysis of the prognostic indexes we only observed a statistically significant difference by chi squared p=0.004 for TRM between patients with ECOG >2 (100% died due to TRM) and patients <2 (28.2% died due to TRM). Among the patients with acute leukemia (27/43) the overall mortality at day +100 was 28.5%. 16 out of the 27 deceased were in CR pre-Haplo-HSCT and 11/27 had an active disease. Comparing the survival of both groups by KM we observed 48% survival for the patients receiving the Haplo-HSCT with CR against 22% for the patients receiving Haplo-HSCT with active disease (figure 1b) at 12 months, which was mantained through the third year (p=0.1 not statistically significant due to the small sample size).
Conclusion
Our results revealed ECOG >2 as an independent variable for TRM with statistical signification. Regarding acute leukemias, we were able to rescue 22% patients with refractory disease at 3 years, which agrees with the results previously published, and rises to 50% for patients receiving the Haplo-HSCT with CR.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Haploidentical stem cell transplantation, Mortality, Transplant-related mortality
Abstract: PB2457
Type: Publication Only
Background
The allogenic stem cell transplantation (Allo-HSCT) is an efficient treatment for patients with high risk hematologic malignancies. Over the past decades new modalities of Allo-HSCT as Haploidentical stem cell transplantation (Haplo-HSCT) allowed us to offer this therapy to patients who for race reasons, presence of rare haplotypes or rapidly progressive disease course can’t find a compatible unrelated donor.
Aims
The aim of this study is to assess the efficacy of Haplo-HSCT on our series evaluating the survival (S), overall mortality (OM) at 100 days and transplant related mortality (TRM).
Methods
We analyzed all the consecutive Haplo-HSCT performed in our center since 2013. The conditioning regimens were decided regarding age, comorbidities and pre-Haplo-HSCT disease status. All patients received high doses of Cy (50 mg/kg on days 3 and 4 posttransplantation) cyclosporine and MMF as CGvHD prophylaxis. We classified the patients before the Haplo-HSCT according to performance status (ECOG), comorbidities (Sorror), disease status (DRI and EBMT). We used SPSS V.23 to calculate the S and OM by the KM test and Chi squared tests.
Results
We performed 43 haplo-HSCT, 25 were males and 18 females with a mean age of 43 (range 16- 68). Diagnosis: Acute myeloid leukemia (24), Acute lymphoid leukemia (3), Hodgkin disease (65), Non Hodgkin lymphoma (2), severe aplastic anemia (2) Chronic lymphoproliferative disease (3). 23/43 patients died throughout the follow-up period with 31% OM at day +100 (fig. 1a). 15/23 patients died due to TRM. 7/8 of the remaining patients died due to disease progression and 5 out of these 7 patients had an active disease pre-Haplo-HSCT. For the analysis of the prognostic indexes we only observed a statistically significant difference by chi squared p=0.004 for TRM between patients with ECOG >2 (100% died due to TRM) and patients <2 (28.2% died due to TRM). Among the patients with acute leukemia (27/43) the overall mortality at day +100 was 28.5%. 16 out of the 27 deceased were in CR pre-Haplo-HSCT and 11/27 had an active disease. Comparing the survival of both groups by KM we observed 48% survival for the patients receiving the Haplo-HSCT with CR against 22% for the patients receiving Haplo-HSCT with active disease (figure 1b) at 12 months, which was mantained through the third year (p=0.1 not statistically significant due to the small sample size).
Conclusion
Our results revealed ECOG >2 as an independent variable for TRM with statistical signification. Regarding acute leukemias, we were able to rescue 22% patients with refractory disease at 3 years, which agrees with the results previously published, and rises to 50% for patients receiving the Haplo-HSCT with CR.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Haploidentical stem cell transplantation, Mortality, Transplant-related mortality


