
Contributions
Abstract: PB2465
Type: Publication Only
Background
It's well known that the disease status before allogeneic stem cell transplantation (allo-HSCT) affects the outcome in adults with acute myeloid leukemia (AML). Multicolor flow cytometry (MFC) is one of the most applicable diagnostic methods to evaluate minimal residual disease (MRD). However, a primary immunophenotype of leukemia cells is often unknown, so the “different from normal” approach to assess MRD could be used in this situation before allo-HSCT.
Aims
To evaluate an impact of MRD by MFC on disease free survival in AML patients after allo-HSCT.
Methods
MRD status was evaluated in 37 patients with AML. All patients received allo-HSCT in National research center for Hematology between September 2015 and December 2017. A median age was 40 years old (19-66 years). There were 14 males and 23 females. All patients had first complete remission (CR1) confirmed by bone marrow morphology. Patients received allo-HSCT from related (n=16) or unrelated (n=21) donors. The intensity of conditioning was mainly reduced (n = 23) rather than myeloablative conditioning (n = 14). Bone marrow (BM) as a graft source was used in 25, PBSC – in 12 pts. MRD was measured before allo-HSCT (2 weeks before conditioning) in bone marrow by 6-color flow cytometry (BD FACS Canto II). The panel of monoclonal antibodies included 4 tubes with core 3 markers (CD33, CD34, CD45) and the set of other markers - CD38, CD13, CD117, CD11b, CD99, CD14, CD16, CD66b, CD65, CD56, HLA-DR. The analysis of MRD was performed based on “different from normal” approach without primary immunophenotype of blast cells. Sensitivity of MFC was 0.01% (50 cells with abnormal immunophenotype from total 500 000 cells). MRD >0,01% was considered as “positive”.
Results
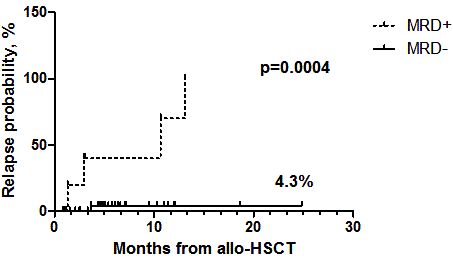
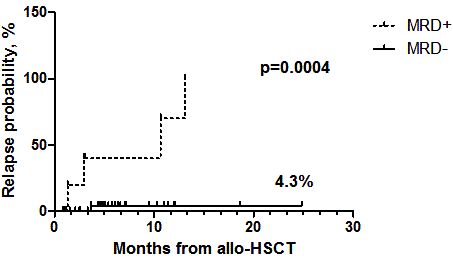
MRD “positivity” before allo-HSCT was detected in 5 patients, MRD “negativity” - in 32. Leukemia relapse was installed in 1 pt in MRD negativity group, 4 in MRD positivity group. Disease free survival in the MRD negativity group was 77,7% versus 32,3% in the MRD “positivity” group, p=0,008. Probability of relapse in MRD ‘‘negativity” and in MRD ‘‘positivity” groups was 76,6% and 4,3%, respectively, p=0,0004 (Fig1).
Conclusion
According to our data MRD analysis based on “different from normal” approach is an effective method for AML patients in CR. Moreover, MRD status before allo-HSCT is an important prognostic factor for detection of a minimal population of blast cells for disease-free survival and can be considered as a discriminator for preemptive or preventive therapy.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Acute Myeloid Leukemia, Allogeneic hematopoietic stem cell transplant, Minimal residual disease (MRD)
Abstract: PB2465
Type: Publication Only
Background
It's well known that the disease status before allogeneic stem cell transplantation (allo-HSCT) affects the outcome in adults with acute myeloid leukemia (AML). Multicolor flow cytometry (MFC) is one of the most applicable diagnostic methods to evaluate minimal residual disease (MRD). However, a primary immunophenotype of leukemia cells is often unknown, so the “different from normal” approach to assess MRD could be used in this situation before allo-HSCT.
Aims
To evaluate an impact of MRD by MFC on disease free survival in AML patients after allo-HSCT.
Methods
MRD status was evaluated in 37 patients with AML. All patients received allo-HSCT in National research center for Hematology between September 2015 and December 2017. A median age was 40 years old (19-66 years). There were 14 males and 23 females. All patients had first complete remission (CR1) confirmed by bone marrow morphology. Patients received allo-HSCT from related (n=16) or unrelated (n=21) donors. The intensity of conditioning was mainly reduced (n = 23) rather than myeloablative conditioning (n = 14). Bone marrow (BM) as a graft source was used in 25, PBSC – in 12 pts. MRD was measured before allo-HSCT (2 weeks before conditioning) in bone marrow by 6-color flow cytometry (BD FACS Canto II). The panel of monoclonal antibodies included 4 tubes with core 3 markers (CD33, CD34, CD45) and the set of other markers - CD38, CD13, CD117, CD11b, CD99, CD14, CD16, CD66b, CD65, CD56, HLA-DR. The analysis of MRD was performed based on “different from normal” approach without primary immunophenotype of blast cells. Sensitivity of MFC was 0.01% (50 cells with abnormal immunophenotype from total 500 000 cells). MRD >0,01% was considered as “positive”.
Results
MRD “positivity” before allo-HSCT was detected in 5 patients, MRD “negativity” - in 32. Leukemia relapse was installed in 1 pt in MRD negativity group, 4 in MRD positivity group. Disease free survival in the MRD negativity group was 77,7% versus 32,3% in the MRD “positivity” group, p=0,008. Probability of relapse in MRD ‘‘negativity” and in MRD ‘‘positivity” groups was 76,6% and 4,3%, respectively, p=0,0004 (Fig1).
Conclusion
According to our data MRD analysis based on “different from normal” approach is an effective method for AML patients in CR. Moreover, MRD status before allo-HSCT is an important prognostic factor for detection of a minimal population of blast cells for disease-free survival and can be considered as a discriminator for preemptive or preventive therapy.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Acute Myeloid Leukemia, Allogeneic hematopoietic stem cell transplant, Minimal residual disease (MRD)


