
Contributions
Abstract: PB1800
Type: Publication Only
Background
Hemophagocytic Lymphohistiocytosis (HLH) is characterized by activation of cytotoxic T-cells and overwhelming cytokine production and release, resulting in an extreme inflammatory response. Primary HLH is most common in children and is genetically driven. Secondary HLH recognises multiple causes, as drugs, autoimmune disease, infection or cancer. Secondary HLH may occur during hematologic neoplasia, as first manifestation of them, before or during the treatment of a recognized malignancy, or associated with relapsing/progressive disease. Hematological malignancy-associated HLH may present an even more severe outcome than primary HLH. Despite the availability of diagnostic criteria, the diagnosis of HLH remains challenging, due to the multiple variables involved and its potential rapidly catastrophic presentation.
Aims
To describe the treatment and outcome of a monocentric, real-life, small cohort of secondary HLH.
Methods
We describe the diagnosis, clinical features, treatment and outcome of five consecutive patients (pts) with secondary HLH presenting at our Centre between March 2016 and December 2017.
Results
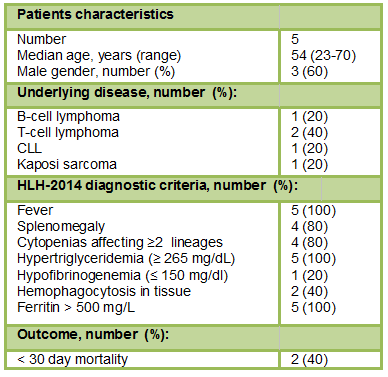
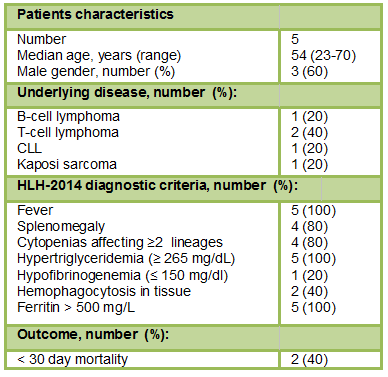
All pts received a diagnosis of HLH based on the HLH-2004 criteria (Table 1). Median age was 54 years (range 23-70), and 3 were male. Associated conditions included hematologic malignancies (80%) and infections (40%). Four pts had hematologic malignancy in relapse (80%): 3 non-Hodgkin lymphoma (B-cell, n=1; T-cell, n=2), 1 CLL. Two pts had also an underlying CMV and EBV viral infection. One patient developed HLH in the setting of Kaposi's sarcoma.
All cases presented with fever, elevated ferritin (≥ 500 µg/l) (median 34.126 µg/l, range 9.130-100.000 µg/l) and high triglycerides (≥265mg/dL)(median 371 mg/dl, range 331-428 mg/dl). Other features at HLH diagnosis were: 4 pts (80%) had splenomegaly, 4 pts (80%) had new onset of ≥ 2 cytopenias, and 1 pt (20%) had low fibrinogen (≤ 150 mg/dl). Bone marrow examination was performed in 3 pts, 2 had morphological evidence of hemophagocytosis (40%). NK-cell activity and sIL2R testing were not performed. The median lactate dehydrogenase (LDH) was 1.784 U/L (range, 458-4.060 U/L). Increase in bilirubin and transaminases or creatinine were seen in 3 and 2 patients, respectively.
All patients received etoposide and dexamethasone treatment, one patient started CHOEP, and one started ibrutinib to control underlying malignancy. One pt received rituximab for EBV infection and one patient received valganciclovir for CMV infection. Two pts died within 30 days from diagnosis, while 3 pts are in HLH CR.
Conclusion
Diagnosis of malignancy-associated HLH in adults is particularly challenging due to the multiplicity of confounding variables and evolution rapidity, possibly leading to a delayed recognition. HLH should be suspected in patients with hematologic malignancies, in particular in T-cell lymphomas, or in the presence of EBV and CMV infections, presenting fever, cytopenias, splenomegaly and ferritin elevated to more than 500 mg/L, that indicate an underlying uncontrolled inflammatory state. A high degree of clinical suspicion allows a prompt diagnosis and treatment, that remain the key factors in the prevention of a HLH catastrophic clinical course.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Ferritin, Fever, Non-Hodgkin's lymphoma
Abstract: PB1800
Type: Publication Only
Background
Hemophagocytic Lymphohistiocytosis (HLH) is characterized by activation of cytotoxic T-cells and overwhelming cytokine production and release, resulting in an extreme inflammatory response. Primary HLH is most common in children and is genetically driven. Secondary HLH recognises multiple causes, as drugs, autoimmune disease, infection or cancer. Secondary HLH may occur during hematologic neoplasia, as first manifestation of them, before or during the treatment of a recognized malignancy, or associated with relapsing/progressive disease. Hematological malignancy-associated HLH may present an even more severe outcome than primary HLH. Despite the availability of diagnostic criteria, the diagnosis of HLH remains challenging, due to the multiple variables involved and its potential rapidly catastrophic presentation.
Aims
To describe the treatment and outcome of a monocentric, real-life, small cohort of secondary HLH.
Methods
We describe the diagnosis, clinical features, treatment and outcome of five consecutive patients (pts) with secondary HLH presenting at our Centre between March 2016 and December 2017.
Results
All pts received a diagnosis of HLH based on the HLH-2004 criteria (Table 1). Median age was 54 years (range 23-70), and 3 were male. Associated conditions included hematologic malignancies (80%) and infections (40%). Four pts had hematologic malignancy in relapse (80%): 3 non-Hodgkin lymphoma (B-cell, n=1; T-cell, n=2), 1 CLL. Two pts had also an underlying CMV and EBV viral infection. One patient developed HLH in the setting of Kaposi's sarcoma.
All cases presented with fever, elevated ferritin (≥ 500 µg/l) (median 34.126 µg/l, range 9.130-100.000 µg/l) and high triglycerides (≥265mg/dL)(median 371 mg/dl, range 331-428 mg/dl). Other features at HLH diagnosis were: 4 pts (80%) had splenomegaly, 4 pts (80%) had new onset of ≥ 2 cytopenias, and 1 pt (20%) had low fibrinogen (≤ 150 mg/dl). Bone marrow examination was performed in 3 pts, 2 had morphological evidence of hemophagocytosis (40%). NK-cell activity and sIL2R testing were not performed. The median lactate dehydrogenase (LDH) was 1.784 U/L (range, 458-4.060 U/L). Increase in bilirubin and transaminases or creatinine were seen in 3 and 2 patients, respectively.
All patients received etoposide and dexamethasone treatment, one patient started CHOEP, and one started ibrutinib to control underlying malignancy. One pt received rituximab for EBV infection and one patient received valganciclovir for CMV infection. Two pts died within 30 days from diagnosis, while 3 pts are in HLH CR.
Conclusion
Diagnosis of malignancy-associated HLH in adults is particularly challenging due to the multiplicity of confounding variables and evolution rapidity, possibly leading to a delayed recognition. HLH should be suspected in patients with hematologic malignancies, in particular in T-cell lymphomas, or in the presence of EBV and CMV infections, presenting fever, cytopenias, splenomegaly and ferritin elevated to more than 500 mg/L, that indicate an underlying uncontrolled inflammatory state. A high degree of clinical suspicion allows a prompt diagnosis and treatment, that remain the key factors in the prevention of a HLH catastrophic clinical course.
Session topic: 21. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Ferritin, Fever, Non-Hodgkin's lymphoma


