
Contributions
Abstract: PB1739
Type: Publication Only
Background
Hyperleukocytosis (HL) is defined as the clinical condition when the white blood cell (WBC) count is above 100 000/mm3 in peripheral blood and the reported incidence of HL is between 5 and 20% in acute myeloid leukemia (AML). The effect of leukapheresis on early mortality data is scarce.
Aims
The aim of this study was to investigate the effect of leukapheresis on early mortality of AML patients with HL
Methods
From January 2005 through October 2017, data from 70 patients with AML who were eligible for leukapheresis were evaluated. All these data were obtained from the Ankara University Faculty of Medicine Center for Therapeutic Apheresis and written informed consent was signed according to our institution regulations. All leukapheresis procedures were performed according to the institutional standard operating procedures after informed consent. Leukapheresis was performed with a continuous-flow blood cell separator (COBE Spectra; TerumoBCT, software version 7.0) via central venous access. The leukapheresis procedures were continued on a daily basis until clinical improvement was determined. Early mortality was defined as death within the first 15 days of leukapheresis.
Results
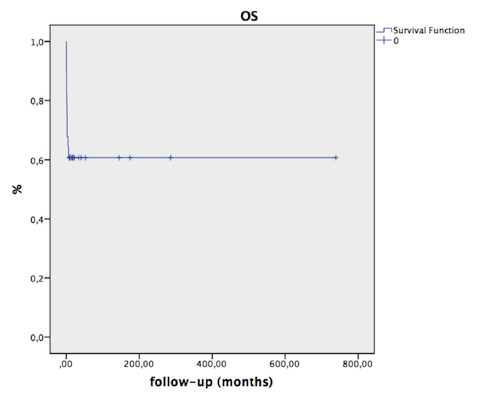
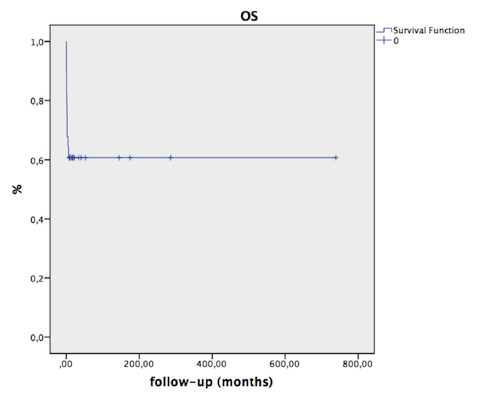
The study cohort consisted of 70 (36 male/33 female) newly diagnosed AML patients who had presented with HL and/or symptoms of leukostasis and underwent leukapheresis. The median age was 52 years (range, 4–86 years). The median WBC counts at diagnosis was 179.2x109/L (range, 56.5-558.0x109/L). The majority of patients, 88.6% (n=62) had WBC count ≥100x109/L. The majority of patients had symptoms of pulmonary leukostasis. A total of 140 leukapheresis cycles were performed among the 70 AML patients. The median number of leukapheresis cycles was 2 (range, 1–7). The median initial WBC was 179.2×109/L, which reduced to 121.7x109/L after the first leukapheresis. Eleven of the seventy patients had died by the time of analysis. Seven patients (10%) died within two weeks after leukapheresis commenced. Among the 7 patients, one patient was treated with induction chemotherapy and the remaining received palliative and supportive care. The main cause of early death was respiratory failure. The mean overall survival for all patients was 112±17 months (95% CI 78–145 months) (Figure). The median overall survival for patients who achieved complete all-cause 2-week mortality rate was 10% (7/70 patients) and the all-cause 4-week mortality rate was 12.8% (9/70 patients).
Conclusion
Leukapheresis is effective and safe procedure in reducing the peripheral blood leukocytes and leukemia blasts. Furthermore, high initial response rates in a subgroup of newly diagnosed AML patients fit to receive intensive chemotherapy suggest that leukapheresis could be beneficial in reducing the complications associated with hyperleukocytosis until systemic intensive chemotherapy commences.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Hyperleukocytosis, Leukapheresis
Abstract: PB1739
Type: Publication Only
Background
Hyperleukocytosis (HL) is defined as the clinical condition when the white blood cell (WBC) count is above 100 000/mm3 in peripheral blood and the reported incidence of HL is between 5 and 20% in acute myeloid leukemia (AML). The effect of leukapheresis on early mortality data is scarce.
Aims
The aim of this study was to investigate the effect of leukapheresis on early mortality of AML patients with HL
Methods
From January 2005 through October 2017, data from 70 patients with AML who were eligible for leukapheresis were evaluated. All these data were obtained from the Ankara University Faculty of Medicine Center for Therapeutic Apheresis and written informed consent was signed according to our institution regulations. All leukapheresis procedures were performed according to the institutional standard operating procedures after informed consent. Leukapheresis was performed with a continuous-flow blood cell separator (COBE Spectra; TerumoBCT, software version 7.0) via central venous access. The leukapheresis procedures were continued on a daily basis until clinical improvement was determined. Early mortality was defined as death within the first 15 days of leukapheresis.
Results
The study cohort consisted of 70 (36 male/33 female) newly diagnosed AML patients who had presented with HL and/or symptoms of leukostasis and underwent leukapheresis. The median age was 52 years (range, 4–86 years). The median WBC counts at diagnosis was 179.2x109/L (range, 56.5-558.0x109/L). The majority of patients, 88.6% (n=62) had WBC count ≥100x109/L. The majority of patients had symptoms of pulmonary leukostasis. A total of 140 leukapheresis cycles were performed among the 70 AML patients. The median number of leukapheresis cycles was 2 (range, 1–7). The median initial WBC was 179.2×109/L, which reduced to 121.7x109/L after the first leukapheresis. Eleven of the seventy patients had died by the time of analysis. Seven patients (10%) died within two weeks after leukapheresis commenced. Among the 7 patients, one patient was treated with induction chemotherapy and the remaining received palliative and supportive care. The main cause of early death was respiratory failure. The mean overall survival for all patients was 112±17 months (95% CI 78–145 months) (Figure). The median overall survival for patients who achieved complete all-cause 2-week mortality rate was 10% (7/70 patients) and the all-cause 4-week mortality rate was 12.8% (9/70 patients).
Conclusion
Leukapheresis is effective and safe procedure in reducing the peripheral blood leukocytes and leukemia blasts. Furthermore, high initial response rates in a subgroup of newly diagnosed AML patients fit to receive intensive chemotherapy suggest that leukapheresis could be beneficial in reducing the complications associated with hyperleukocytosis until systemic intensive chemotherapy commences.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia, Hyperleukocytosis, Leukapheresis


