
Contributions
Abstract: S890
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 17:00 - 17:15
Location: Room A9
Background
Prophylactic therapy with factor concentrates administered 2 to 3 times a week on a regular basis is the gold standard treatment for haemophilia[1]. In countries with limited resources, initiating prophylaxis with very low dose and at reduced frequency could be recommended.
Aims
We report our single centre experience from a Hemophilia Treatment Centre at rural eastern India with very low dose once weekly prophylaxis regimen in children with haemophilia A.
Methods
It was an open label prospective trial using historical data as control. Children with severe haemophilia A, below the age of 15 years, were included. The patients received very low dose prophylaxis with recombinant F-VIII, at the dose of 15 IU/kg once weekly. The dose was approximated to nearest 250 IU or 500 IU F-VIII, for optimal use of Factor vials. The Anti Hemophilic Factors (AHF) were provided by Hemophilia Federation of India on compassionate ground free of cost. The patients were followed up for 6 months (June 2017- November 2017) and clinical and joint evaluation parameters were compared with historical data in previous 6 month period. APTT-based Inhibitor screening was done at study entry and then at the end of 6 month.
Results
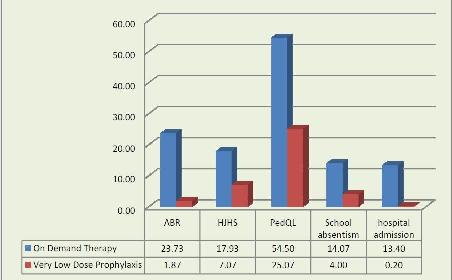
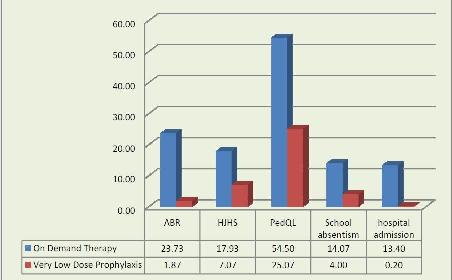
Altogether 18 patients were included in the study, but 3 patients were excluded from calculation, as they discontinued the prophylaxis because of logistics issues. The mean age of patients was 9.47 years (Range 3-15 years) and mean body weight were 28 Kg, (range 12-40 Kg). All the patients were previously exposed to AHF infusion as On Demand Therapy. There was significant reduction of ABR during prophylaxis therapy (23.73 before prophylaxis vs 1.87 after prophylaxis, P value <0.001). Similarly, no. of days of hospitalisation for rescue therapy was also reduced significantly. No patient developed inhibitor during the study period. The Social and functional parameters like PedQL score and days of school absenteeism also reduced significantly. The AHF use was about 1235 IU/Kg/year during on demand therapy, which came down to 821 IU/Kg/year during prophylaxis.
Conclusion
Prophylaxis in haemophilia is a big challenge in resource constrained developing countries. Also the limited access to haemophilia treatment centre in rural India, difficulty in using public transport facility by haemophiliacs and lack of knowledge about self infusion and home based therapy makes prophylaxis program more difficult. The very low dose prophylaxis regimen of 15 units/kg once a week AHF was quite convenient and acceptable to the children with haemophilia. It is effective in preventing joint bleeds and overall bleeds and also is cost effective. Significantly less emergency visits, lesser days of school absenteeism and improved quality of life can be achieved in children with very low dose prophylaxis.
Session topic: 34. Bleeding disorders (congenital and acquired)
Abstract: S890
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 17:00 - 17:15
Location: Room A9
Background
Prophylactic therapy with factor concentrates administered 2 to 3 times a week on a regular basis is the gold standard treatment for haemophilia[1]. In countries with limited resources, initiating prophylaxis with very low dose and at reduced frequency could be recommended.
Aims
We report our single centre experience from a Hemophilia Treatment Centre at rural eastern India with very low dose once weekly prophylaxis regimen in children with haemophilia A.
Methods
It was an open label prospective trial using historical data as control. Children with severe haemophilia A, below the age of 15 years, were included. The patients received very low dose prophylaxis with recombinant F-VIII, at the dose of 15 IU/kg once weekly. The dose was approximated to nearest 250 IU or 500 IU F-VIII, for optimal use of Factor vials. The Anti Hemophilic Factors (AHF) were provided by Hemophilia Federation of India on compassionate ground free of cost. The patients were followed up for 6 months (June 2017- November 2017) and clinical and joint evaluation parameters were compared with historical data in previous 6 month period. APTT-based Inhibitor screening was done at study entry and then at the end of 6 month.
Results
Altogether 18 patients were included in the study, but 3 patients were excluded from calculation, as they discontinued the prophylaxis because of logistics issues. The mean age of patients was 9.47 years (Range 3-15 years) and mean body weight were 28 Kg, (range 12-40 Kg). All the patients were previously exposed to AHF infusion as On Demand Therapy. There was significant reduction of ABR during prophylaxis therapy (23.73 before prophylaxis vs 1.87 after prophylaxis, P value <0.001). Similarly, no. of days of hospitalisation for rescue therapy was also reduced significantly. No patient developed inhibitor during the study period. The Social and functional parameters like PedQL score and days of school absenteeism also reduced significantly. The AHF use was about 1235 IU/Kg/year during on demand therapy, which came down to 821 IU/Kg/year during prophylaxis.
Conclusion
Prophylaxis in haemophilia is a big challenge in resource constrained developing countries. Also the limited access to haemophilia treatment centre in rural India, difficulty in using public transport facility by haemophiliacs and lack of knowledge about self infusion and home based therapy makes prophylaxis program more difficult. The very low dose prophylaxis regimen of 15 units/kg once a week AHF was quite convenient and acceptable to the children with haemophilia. It is effective in preventing joint bleeds and overall bleeds and also is cost effective. Significantly less emergency visits, lesser days of school absenteeism and improved quality of life can be achieved in children with very low dose prophylaxis.
Session topic: 34. Bleeding disorders (congenital and acquired)


