
Contributions
Abstract: S126
Type: Oral Presentation
Presentation during EHA23: On Friday, June 15, 2018 from 12:00 - 12:15
Location: Room A6
Background
Contemporary practice in allogeneic stem cell transplantation (SCT) has increased the likelihood of finding donors for nearly all transplantation candidates. Furthermore, older patients (pts) are being transplanted.
Aims
We sought to explore the relationship between increasing age, donor selection, and risk of non-relapse mortality (NRM).
Methods
A retrospective study including 55,941 adult pts treated for hematologic malignancies who underwent first SCT from sibling (MSD), matched (MUD) or mismatched (MMUD) unrelated, cord blood (CB) or haploidentical (Haplo) donors between 2010 and 2015 in European Society for Blood and Marrow Transplantation (EBMT) centers. We compared outcomes across four consecutive age groups (18-39 [I], 40-49 [II], 50-59 [III], >=60 [IV]). The primary outcome was NRM. Within each age group, using a Cox regression model adjusted for key variables, we studied the risk associated with different donor types. MSDs were the reference category.
Results
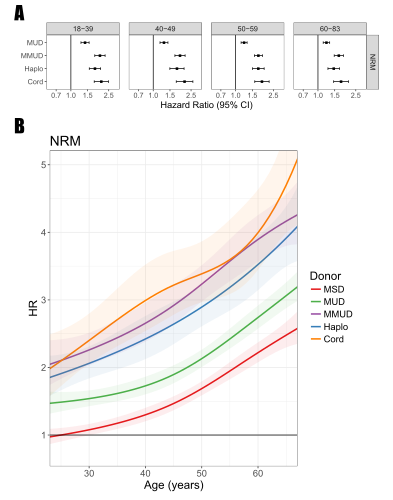
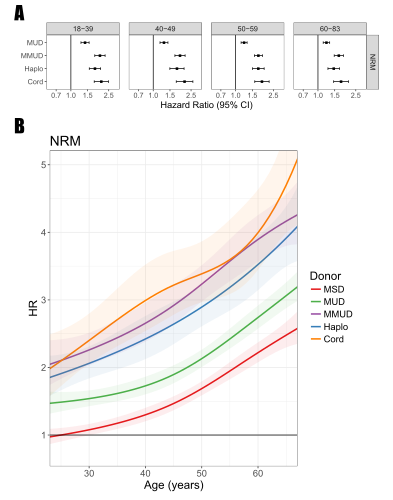
Younger patients were more likely to receive MSD grafts (39% [group I], 39% [II], 38% [III], and 26% [IV]) and myeloablative conditioning (76% [I], 61% [II], 40% [III], and 23 [IV]. Unrelated donors were increasingly used with increasing age (49% [I], 53% [II], 56% [III], 66% [IV]). Haplo and CB transplant were more prevalent in ages 18-39 (9% and 4%, respectively), compared to all other age groups. The probability of 3-year NRM increased with age, regardless of donor type. (Table). Across all age groups, NRM was lowest with MSD followed by MUD and Haplo, while the highest incidence was in transplants from MMUD and CB. 3-year overall survival (OS) was also higher with MSDs and MUDs in all age groups. Notably, among older pts (group IV) receiving grafts from alternative donors, Haplo was associated with better OS (38.5%) compared to MMUD (33.1%) and CB (22.9%). MUD transplants had increased risk for NRM compared to MSDs regardless of age group (HR ranging from 1.2 to 1.4, Figure 1a). Alternative donors had an overlapping risk for NRM ranging from 1.5-2.1 (reference MSD). Using cubic splines, we further validated these findings by modeling the risk of donors across age as a continuous factor (Figure 1b).
| 18-39 | 40-49 | 50-59 | 60-83 | |
3-year Non-Relapse Mortality (95% CI)
| MSD | 15.8 (14.7-17.0) | 19.7 (18.4-21.1) | 24.3 (23.1-25.6) | 28.5 (26.9-30.2) |
MUD | 21.9 (20.5-23.4) | 24.4 (22.8-26.1) | 29.4 (28.0-30.8) | 34.5 (33.1-36.0) | |
Haplo | 25.8 (23.2-28.6) | 32.0 (28.0-36.5) | 36.0 (32.4-40.0) | 38.9 (35.2-42.9) | |
MMUD | 30.8 (28.1-33.7) | 34.5 (31.4-38.0) | 39.8 (37.1-42.8) | 44.0 (41.1-47.2) | |
Cord | 30.4 (26.6-34.6) | 35.8 (30.7-41.7) | 39.2 (34.3-44.8) | 43.9 (38.6-50.0) | |
3-year Overall Survival (95% CI)
| MSD | 59.8 (58.1-61.4) | 58.4 (56.7-60.2) | 52.4 (50.9-54.0) | 45.3 (43.5-47.3) |
MUD | 59.4 (57.6-61.2) | 55.6 (53.6-57.6) | 49.5 (47.9-51.1) | 44.5 (43.0-46.0) | |
Haplo | 49.8 (46.7-53.1) | 42.6 (38.1-47.6) | 41.5 (37.6-45.8) | 38.5 (34.6-42.7) | |
MMUD | 47.5 (44.5-50.8) | 44.2 (40.7-47.9) | 41.1 (38.3-44.2) | 33.1 (30.2-36.2) | |
Cord | 25.5 (21.9-29.6) | 32.3 (27.2-38.2) | 26.7 (22.3-31.9) | 22.9 (18.5-28.5) | |
Conclusion
MSDs remains the safest option in all age groups. In older pts with no conventional donor available, Haplo may be preferable because of reduced NRM in comparison to MMUD and CB.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Allogeneic hematopoietic stem cell transplant, Donor, Mortality
Abstract: S126
Type: Oral Presentation
Presentation during EHA23: On Friday, June 15, 2018 from 12:00 - 12:15
Location: Room A6
Background
Contemporary practice in allogeneic stem cell transplantation (SCT) has increased the likelihood of finding donors for nearly all transplantation candidates. Furthermore, older patients (pts) are being transplanted.
Aims
We sought to explore the relationship between increasing age, donor selection, and risk of non-relapse mortality (NRM).
Methods
A retrospective study including 55,941 adult pts treated for hematologic malignancies who underwent first SCT from sibling (MSD), matched (MUD) or mismatched (MMUD) unrelated, cord blood (CB) or haploidentical (Haplo) donors between 2010 and 2015 in European Society for Blood and Marrow Transplantation (EBMT) centers. We compared outcomes across four consecutive age groups (18-39 [I], 40-49 [II], 50-59 [III], >=60 [IV]). The primary outcome was NRM. Within each age group, using a Cox regression model adjusted for key variables, we studied the risk associated with different donor types. MSDs were the reference category.
Results
Younger patients were more likely to receive MSD grafts (39% [group I], 39% [II], 38% [III], and 26% [IV]) and myeloablative conditioning (76% [I], 61% [II], 40% [III], and 23 [IV]. Unrelated donors were increasingly used with increasing age (49% [I], 53% [II], 56% [III], 66% [IV]). Haplo and CB transplant were more prevalent in ages 18-39 (9% and 4%, respectively), compared to all other age groups. The probability of 3-year NRM increased with age, regardless of donor type. (Table). Across all age groups, NRM was lowest with MSD followed by MUD and Haplo, while the highest incidence was in transplants from MMUD and CB. 3-year overall survival (OS) was also higher with MSDs and MUDs in all age groups. Notably, among older pts (group IV) receiving grafts from alternative donors, Haplo was associated with better OS (38.5%) compared to MMUD (33.1%) and CB (22.9%). MUD transplants had increased risk for NRM compared to MSDs regardless of age group (HR ranging from 1.2 to 1.4, Figure 1a). Alternative donors had an overlapping risk for NRM ranging from 1.5-2.1 (reference MSD). Using cubic splines, we further validated these findings by modeling the risk of donors across age as a continuous factor (Figure 1b).
| 18-39 | 40-49 | 50-59 | 60-83 | |
3-year Non-Relapse Mortality (95% CI)
| MSD | 15.8 (14.7-17.0) | 19.7 (18.4-21.1) | 24.3 (23.1-25.6) | 28.5 (26.9-30.2) |
MUD | 21.9 (20.5-23.4) | 24.4 (22.8-26.1) | 29.4 (28.0-30.8) | 34.5 (33.1-36.0) | |
Haplo | 25.8 (23.2-28.6) | 32.0 (28.0-36.5) | 36.0 (32.4-40.0) | 38.9 (35.2-42.9) | |
MMUD | 30.8 (28.1-33.7) | 34.5 (31.4-38.0) | 39.8 (37.1-42.8) | 44.0 (41.1-47.2) | |
Cord | 30.4 (26.6-34.6) | 35.8 (30.7-41.7) | 39.2 (34.3-44.8) | 43.9 (38.6-50.0) | |
3-year Overall Survival (95% CI)
| MSD | 59.8 (58.1-61.4) | 58.4 (56.7-60.2) | 52.4 (50.9-54.0) | 45.3 (43.5-47.3) |
MUD | 59.4 (57.6-61.2) | 55.6 (53.6-57.6) | 49.5 (47.9-51.1) | 44.5 (43.0-46.0) | |
Haplo | 49.8 (46.7-53.1) | 42.6 (38.1-47.6) | 41.5 (37.6-45.8) | 38.5 (34.6-42.7) | |
MMUD | 47.5 (44.5-50.8) | 44.2 (40.7-47.9) | 41.1 (38.3-44.2) | 33.1 (30.2-36.2) | |
Cord | 25.5 (21.9-29.6) | 32.3 (27.2-38.2) | 26.7 (22.3-31.9) | 22.9 (18.5-28.5) | |
Conclusion
MSDs remains the safest option in all age groups. In older pts with no conventional donor available, Haplo may be preferable because of reduced NRM in comparison to MMUD and CB.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Allogeneic hematopoietic stem cell transplant, Donor, Mortality


