
Contributions
Abstract: S874
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 16:45 - 17:00
Location: Room A6
Background
Autologous stem cell transplantation (ASCT) has been proposed as consolidation therapy for patients with acute myeloid leukemia (AML). Concern regarding the risk of relapse has led to decreasing use of this procedure. However, ASCT has been shown to be a putative strategy for reducing relapse and is associated with reduced non-relapse mortality (NRM) and a better quality of life compared to allogeneic SCT.
Aims
Develop a prediction model for Leukemia Free Survival (LFS) in AML patients treated with an ASCT.
Methods
This was a retrospective study of adult AML patients in complete remission (CR), treated with ASCT as consolidation therapy between 2000 and 2015 in European Society for Blood and Marrow Transplantation (EBMT) centers. The primary outcome was LFS, defined as death or relapse following ASCT. To develop a nomogram for prediction of 3-year and 5-year, we first performed a univariate analysis, introducing statistically significant (p<0.1) variables into a Cox regression multivariable model. The final model was chosen according to the Akaike information criterion. The performance was assessed using time-dependent c-statistic.
Results
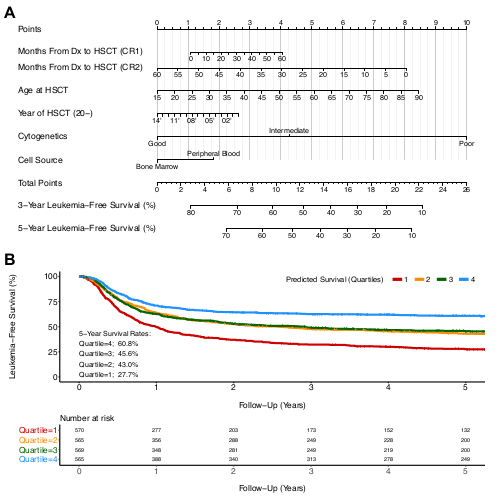
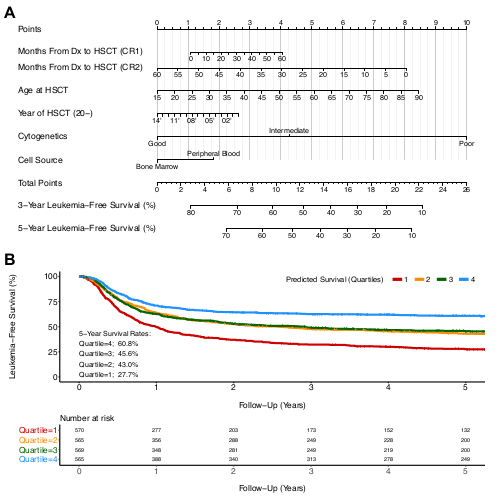
A total of 2,298 AML pts, with a median age of 49 (IQR: 38-58) were included. The majority of pts were in CR1 (90%) and had intermediate risk cytogenetics (75%), followed by good (18.5%), and poor (6.5%). Peripheral blood was the cell source in 93% of the cases. TBI was used as the backbone of conditioning in 86% of the pts. The final variables included in the multivariable model were age, cytogenetic risk group (Medical Research Council classification), cell source, year of transplantation, and disease status and time from diagnosis to transplantation as an interaction term. The nomogram is present in Figure 1a. The cumulative points a patient receives corresponds with 3-year and 5-year LFS probability, described in the bottom rows. Prognostic discrimination was performed by dividing the predicted survival probabilities into quartiles that were then used to plot Kaplan-Meier curves (Figure 1b). Patients in the highest and lowest quartiles had a 60.8% and 27.7% probability of 5-year LFS. The c-statistic of the model for 5-year LFS was 0.64.
Conclusion
We present the first predictive score for AML patients treated with ASCT. The score may help to better define patients who benefit from autologous transplantation as post-remission treatment.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Acute Myeloid Leukemia, Autologous hematopoietic stem cell transplantation, Prediction
Abstract: S874
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 16:45 - 17:00
Location: Room A6
Background
Autologous stem cell transplantation (ASCT) has been proposed as consolidation therapy for patients with acute myeloid leukemia (AML). Concern regarding the risk of relapse has led to decreasing use of this procedure. However, ASCT has been shown to be a putative strategy for reducing relapse and is associated with reduced non-relapse mortality (NRM) and a better quality of life compared to allogeneic SCT.
Aims
Develop a prediction model for Leukemia Free Survival (LFS) in AML patients treated with an ASCT.
Methods
This was a retrospective study of adult AML patients in complete remission (CR), treated with ASCT as consolidation therapy between 2000 and 2015 in European Society for Blood and Marrow Transplantation (EBMT) centers. The primary outcome was LFS, defined as death or relapse following ASCT. To develop a nomogram for prediction of 3-year and 5-year, we first performed a univariate analysis, introducing statistically significant (p<0.1) variables into a Cox regression multivariable model. The final model was chosen according to the Akaike information criterion. The performance was assessed using time-dependent c-statistic.
Results
A total of 2,298 AML pts, with a median age of 49 (IQR: 38-58) were included. The majority of pts were in CR1 (90%) and had intermediate risk cytogenetics (75%), followed by good (18.5%), and poor (6.5%). Peripheral blood was the cell source in 93% of the cases. TBI was used as the backbone of conditioning in 86% of the pts. The final variables included in the multivariable model were age, cytogenetic risk group (Medical Research Council classification), cell source, year of transplantation, and disease status and time from diagnosis to transplantation as an interaction term. The nomogram is present in Figure 1a. The cumulative points a patient receives corresponds with 3-year and 5-year LFS probability, described in the bottom rows. Prognostic discrimination was performed by dividing the predicted survival probabilities into quartiles that were then used to plot Kaplan-Meier curves (Figure 1b). Patients in the highest and lowest quartiles had a 60.8% and 27.7% probability of 5-year LFS. The c-statistic of the model for 5-year LFS was 0.64.
Conclusion
We present the first predictive score for AML patients treated with ASCT. The score may help to better define patients who benefit from autologous transplantation as post-remission treatment.
Session topic: 23. Stem cell transplantation - Clinical
Keyword(s): Acute Myeloid Leukemia, Autologous hematopoietic stem cell transplantation, Prediction


