
Contributions
Abstract: S857
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 16:00 - 16:15
Location: Room A2
Background
This is the 1st report of the planned analysis of donor availability and outcome in the E2906 phase III trial of intensive therapy in patients (pts) age ≥60 years with newly-diagnosed AML.
Aims
Determine availability of HLA-matched donor and its impact on relapse & survival from 1st remission in the E2906 prospective study of ‘curative’ therapy with integrated allogeneic transplantation (AlloBMT).
Methods
727 pts were registered (2011-2015) to receive induction therapy on E2906, with results previously presented (Foran, ASH 2015, #217). All pts in 1st ‘remission’ [complete remission (CR), CRi (platelets (plts) <100K), or leukemia-free state] with 10/10 HLA-matched donor were eligible for protocol AlloBMT using a busulfan-fludarabine reduced intensity conditioning (RIC) regimen. Living siblings, intent to initiate donor search, & comorbidity (HCT-CI) score at AML diagnosis was recorded for all pts. Survival from remission was determined by Kaplan-Meier method, and we performed a multivariate analysis using Cox models to determine impact of matched donor availability on Overall (OS) & Leukemia-Free survival (LFS; relapse or death from remission) with established AML risk factors.
Results
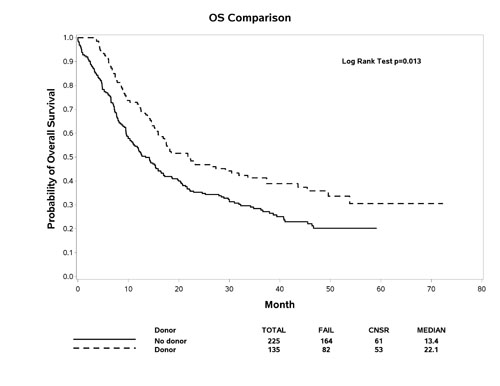
360 patients in ‘remission’ (centrally reviewed) were included in this pre-specified analysis; 135 (37.5%) had a donor identified (sibling 42%, unrelated 58%), & 225 did not. Patients with donor were more likely baseline age<70yrs (p<0.01), performance status (PS)=0 (p=0.03), & plts≥50K (p<0.01). 61/135 (45%) underwent protocol-specified RIC AlloBMT in 1st remission, and 55 additional pts underwent non-protocol AlloBMT, including 25 in the No Donor group. The median follow-up is 37.7 months, and OS by Donor status is noted in Figure (p=0.013). On multivariate analysis, favorable risk cytogen., PS, & plts≥50K were significantly associated with OS (Table). After stratification by age, secondary (vs. de novo) AML & induction treatment, and adjusted for cytogenetics, plts, PS & HCT-CI, availability of matched Donor was associated with 24% reduction OS risk, however did not meet statistical significance on multivariate analysis (HR: 0.76, 95% CI [0.56, 1.04], p=0.09). Similar results were observed for LFS in multivariate model (HR: 0.76, 95% CI [0.56, 1.03], p=0.07).
Multivariate Cox Model – OS | P Value | Hazard Ratio (HR) | 95% HR CI | |
Donor vs. No donor | 0.09 | 0.76 | 0.56 | 1.04 |
Baseline HCT-CI 0 vs. >2 | 0.33 | 0.82 | 0.56 | 1.22 |
Favorable vs. Unfavorable Risk Cytogenetics | 0.002 | 0.25 | 0.11 | 0.59 |
Platelet <50K vs. ≥50K | <.0001 | 1.89 | 1.39 | 2.55 |
Performance status 2 vs. 0 | 0.02 | 1.68 | 1.07 | 2.63 |
Performance status 3 vs. 0 | 0.004 | 5.32 | 1.70 | 16.65 |
Unfavorable Risk Cytogen., Donor vs. No Donor | 0.13 | 0.65 | 0.38 | 1.13 |
Conclusion
An OS advantage was observed in this 1st prospective Donor vs. No Donor analysis from E2906 in older adults, although matched donor status was not significant in the multivariate model. Further analysis is being performed to identify barriers to AlloBMT in this population, and its impact in CR1 vs. conventional therapy.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Allogeneic hematopoietic stem cell transplant, AML, HLA, Survival
Abstract: S857
Type: Oral Presentation
Presentation during EHA23: On Saturday, June 16, 2018 from 16:00 - 16:15
Location: Room A2
Background
This is the 1st report of the planned analysis of donor availability and outcome in the E2906 phase III trial of intensive therapy in patients (pts) age ≥60 years with newly-diagnosed AML.
Aims
Determine availability of HLA-matched donor and its impact on relapse & survival from 1st remission in the E2906 prospective study of ‘curative’ therapy with integrated allogeneic transplantation (AlloBMT).
Methods
727 pts were registered (2011-2015) to receive induction therapy on E2906, with results previously presented (Foran, ASH 2015, #217). All pts in 1st ‘remission’ [complete remission (CR), CRi (platelets (plts) <100K), or leukemia-free state] with 10/10 HLA-matched donor were eligible for protocol AlloBMT using a busulfan-fludarabine reduced intensity conditioning (RIC) regimen. Living siblings, intent to initiate donor search, & comorbidity (HCT-CI) score at AML diagnosis was recorded for all pts. Survival from remission was determined by Kaplan-Meier method, and we performed a multivariate analysis using Cox models to determine impact of matched donor availability on Overall (OS) & Leukemia-Free survival (LFS; relapse or death from remission) with established AML risk factors.
Results
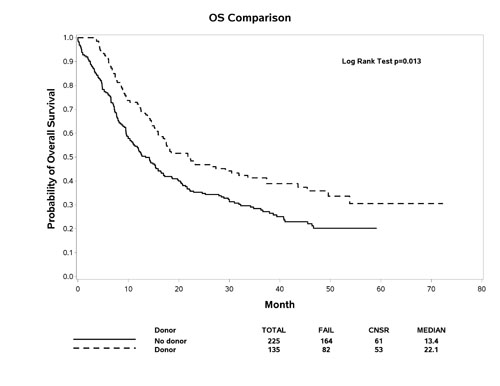
360 patients in ‘remission’ (centrally reviewed) were included in this pre-specified analysis; 135 (37.5%) had a donor identified (sibling 42%, unrelated 58%), & 225 did not. Patients with donor were more likely baseline age<70yrs (p<0.01), performance status (PS)=0 (p=0.03), & plts≥50K (p<0.01). 61/135 (45%) underwent protocol-specified RIC AlloBMT in 1st remission, and 55 additional pts underwent non-protocol AlloBMT, including 25 in the No Donor group. The median follow-up is 37.7 months, and OS by Donor status is noted in Figure (p=0.013). On multivariate analysis, favorable risk cytogen., PS, & plts≥50K were significantly associated with OS (Table). After stratification by age, secondary (vs. de novo) AML & induction treatment, and adjusted for cytogenetics, plts, PS & HCT-CI, availability of matched Donor was associated with 24% reduction OS risk, however did not meet statistical significance on multivariate analysis (HR: 0.76, 95% CI [0.56, 1.04], p=0.09). Similar results were observed for LFS in multivariate model (HR: 0.76, 95% CI [0.56, 1.03], p=0.07).
Multivariate Cox Model – OS | P Value | Hazard Ratio (HR) | 95% HR CI | |
Donor vs. No donor | 0.09 | 0.76 | 0.56 | 1.04 |
Baseline HCT-CI 0 vs. >2 | 0.33 | 0.82 | 0.56 | 1.22 |
Favorable vs. Unfavorable Risk Cytogenetics | 0.002 | 0.25 | 0.11 | 0.59 |
Platelet <50K vs. ≥50K | <.0001 | 1.89 | 1.39 | 2.55 |
Performance status 2 vs. 0 | 0.02 | 1.68 | 1.07 | 2.63 |
Performance status 3 vs. 0 | 0.004 | 5.32 | 1.70 | 16.65 |
Unfavorable Risk Cytogen., Donor vs. No Donor | 0.13 | 0.65 | 0.38 | 1.13 |
Conclusion
An OS advantage was observed in this 1st prospective Donor vs. No Donor analysis from E2906 in older adults, although matched donor status was not significant in the multivariate model. Further analysis is being performed to identify barriers to AlloBMT in this population, and its impact in CR1 vs. conventional therapy.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Allogeneic hematopoietic stem cell transplant, AML, HLA, Survival


