
Contributions
Abstract: S147
Type: Oral Presentation
Presentation during EHA23: On Friday, June 15, 2018 from 12:15 - 12:30
Location: Room A10
Background
Light-chain (AL) amyloidosis is a rare, progressive and typically fatal disease in which misfolded light chains are deposited in tissues and organs, which may lead to organ failure, disability, and death. The cardiac biomarker B-type natriuretic peptide (BNP) or N-terminal pro B-type natriuretic peptide (NT-proBNP) is used to monitor disease progression and response to treatment among patients with cardiac involvement from AL amyloidosis. The relationships between these cardiac biomarkers and health-related quality of life (HRQoL) are poorly understood in this condition.
Aims
To examine whether HRQoL in patients with cardiac AL amyloidosis differs significantly by changes in BNP or NT-proBNP.
Methods
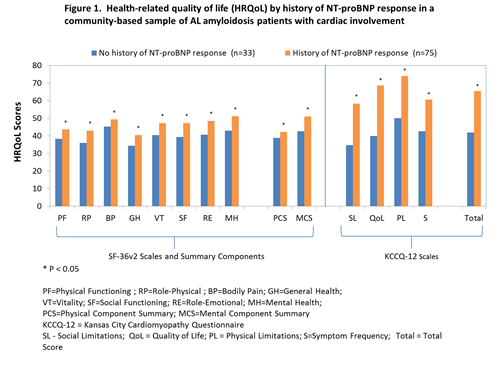
We obtained cardiac biomarker and HRQoL data from AL amyloidosis patients from two data sources: a community-based sample (n=108) and a clinical sample of patients seen at the Amyloidosis Center at Boston University School of Medicine at Boston Medical Center (n=95). In the community-based sample, HRQoL scores (based on the SF-36® Health Survey [SF-36] and the Kansas City Cardiomyopathy Short Form [KCCQ-12]) were examined by patients with and without a self-reported decline in NT-proBNP ≥ 30%. Separate generalized linear models, adjusted for complete hematologic response, were used to compare HRQoL scores by NT-proBNP response to treatment. HRQoL scores were reported relative to existing benchmarks, including: 1) mean SF-36 scores from both a general population sample and patients with congestive heart failure (CHF); 2) mean KCCQ scores according to New York Heart Association functional classes. Analysis of variance was used to compare SF-36 scores to age- and gender- adjusted benchmarks.
In the clinical sample, both pre- and post-treatment SF-36 scores and BNP lab values were obtained from medical record reviews. Generalized linear models, controlling for baseline SF-36 scores, were used to test for significant differences in SF-36 change scores among patients with and without a decline in BNP ≥ 30%.
Results
In the community-based sample, patients with an NT-proBNP response had significantly better HRQoL than those without for all SF-36 and KCCQ scales and summary scores (P < 0.05 for all; Figure 1). Patients without an NT-proBNP response had SF-36 scores that were comparable to CHF benchmarks. Analyses in the clinical sample further supported longitudinal associations between changes in cardiac biomarkers and changes in SF-36 scores.
Conclusion
This study provided consistent preliminary evidence of a relationship between cardiac biomarkers and HRQoL using multiple data sources and different analytic approaches. These findings should be replicated in larger, longitudinal samples. A clearer understanding of the relationship between these frequently-used biomarkers and HRQoL can aid those in the scientific community who want to continue using these biomarkers to develop prognoses, evaluate treatment efficacy, and develop relevant and meaningful endpoints for clinical trials in patients with AL amyloidosis.
Session topic: 36. Quality of life, palliative care, ethics and health economics
Keyword(s): AL amyloidosis, Quality of Life
Abstract: S147
Type: Oral Presentation
Presentation during EHA23: On Friday, June 15, 2018 from 12:15 - 12:30
Location: Room A10
Background
Light-chain (AL) amyloidosis is a rare, progressive and typically fatal disease in which misfolded light chains are deposited in tissues and organs, which may lead to organ failure, disability, and death. The cardiac biomarker B-type natriuretic peptide (BNP) or N-terminal pro B-type natriuretic peptide (NT-proBNP) is used to monitor disease progression and response to treatment among patients with cardiac involvement from AL amyloidosis. The relationships between these cardiac biomarkers and health-related quality of life (HRQoL) are poorly understood in this condition.
Aims
To examine whether HRQoL in patients with cardiac AL amyloidosis differs significantly by changes in BNP or NT-proBNP.
Methods
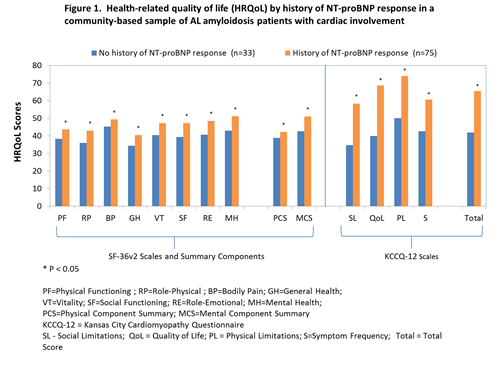
We obtained cardiac biomarker and HRQoL data from AL amyloidosis patients from two data sources: a community-based sample (n=108) and a clinical sample of patients seen at the Amyloidosis Center at Boston University School of Medicine at Boston Medical Center (n=95). In the community-based sample, HRQoL scores (based on the SF-36® Health Survey [SF-36] and the Kansas City Cardiomyopathy Short Form [KCCQ-12]) were examined by patients with and without a self-reported decline in NT-proBNP ≥ 30%. Separate generalized linear models, adjusted for complete hematologic response, were used to compare HRQoL scores by NT-proBNP response to treatment. HRQoL scores were reported relative to existing benchmarks, including: 1) mean SF-36 scores from both a general population sample and patients with congestive heart failure (CHF); 2) mean KCCQ scores according to New York Heart Association functional classes. Analysis of variance was used to compare SF-36 scores to age- and gender- adjusted benchmarks.
In the clinical sample, both pre- and post-treatment SF-36 scores and BNP lab values were obtained from medical record reviews. Generalized linear models, controlling for baseline SF-36 scores, were used to test for significant differences in SF-36 change scores among patients with and without a decline in BNP ≥ 30%.
Results
In the community-based sample, patients with an NT-proBNP response had significantly better HRQoL than those without for all SF-36 and KCCQ scales and summary scores (P < 0.05 for all; Figure 1). Patients without an NT-proBNP response had SF-36 scores that were comparable to CHF benchmarks. Analyses in the clinical sample further supported longitudinal associations between changes in cardiac biomarkers and changes in SF-36 scores.
Conclusion
This study provided consistent preliminary evidence of a relationship between cardiac biomarkers and HRQoL using multiple data sources and different analytic approaches. These findings should be replicated in larger, longitudinal samples. A clearer understanding of the relationship between these frequently-used biomarkers and HRQoL can aid those in the scientific community who want to continue using these biomarkers to develop prognoses, evaluate treatment efficacy, and develop relevant and meaningful endpoints for clinical trials in patients with AL amyloidosis.
Session topic: 36. Quality of life, palliative care, ethics and health economics
Keyword(s): AL amyloidosis, Quality of Life


