
Contributions
Abstract: S101
Type: Oral Presentation
Presentation during EHA23: On Friday, June 15, 2018 from 11:45 - 12:00
Location: Room A1
Background
Follicular lymphoma (FL) patients (pts) have high long-term survival probability in majority of cases, however some subgroups especially early progressors and pts with transformation poor outcome. Prognostic indexes could partially help and recently presented PRIMA PI (Bachy ASH2017) is the first one based on population of immunochemotherapy treated pts (PRIMA study).
Aims
Validation of PRIMA PI in large cohort of real world treated pts and analysis of impact of different PRIMA PI risk groups on progression within 24 months since start of therapy (POD24).
Methods
This analysis was part of NiHiL project (GovTrial No: NCT03199066). NiHiL project is based on prospective collection and analysis of diagnostic, epidemiologic and therapeutic data of NHL patients. All patients signed the informed consent approved by EC. The eligibility criteria were: all consecutively pts with confirmed FL dg, with confirmation of essential data (clinical characteristic, therapy, follow-up) treated with immunochemotherapy. Progression free survival (PFS) and Overall survival (OS) were counted since the therapy initiation. Pearson's Chi-square Test was used for group comparison, log rank test for survival analysis.
Results
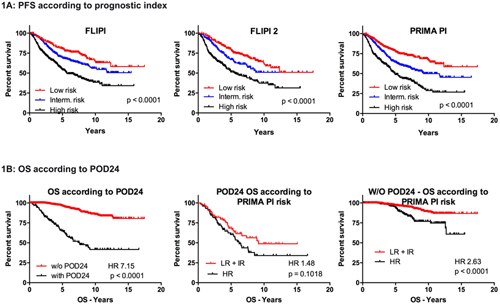
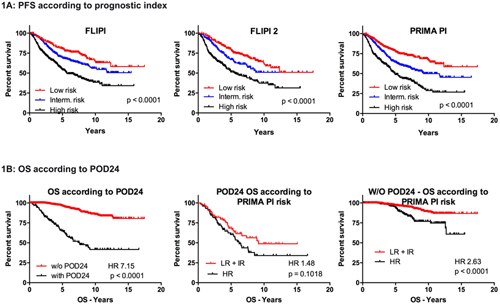
Altogether 1179 pts diagnosed 1999-2015 and treated with immunochemotherapy in 1st line 2000-2015 fulfilled eligibility criteria. The majority (893) had grade 1 or 2, followed by gr 3A (188) or without given grade (98). Median age was 59y (26-87), BM was involved in 50.4% cases, LDH was elevated in 42.1% cases and beta2microglobulin >3mg/l in 31.8% of pts. Low risk group (LRG) according to FLIPI, FLIPI2 and PRIMA PI resp. represent 20.5%, 35.5% and 39.0% pts resp., intermediate risk group (IRG) 31.3%, 25.6% and 29.2% pts resp., high risk group (HRG) 48.1%, 38.9% and 31.8% pts resp. All patients were treated with rituximab and majority of pts (76.3%) were treated with CHOP, CVP was used in 13.3% pts, bendamustine 2.8%, fludarabine 2.6% and the rest with other regimens according to centres policy (PACEBO, sequential protocol and others). ORR (Cheson 1999) was reached in 92.4% of pts, out of these 66.7% received rituximab maintenance. With the median follow-up 6.1y there was 7y PFS and OS probability 58.7% and 82.3%. According to FLIPI, FLIPI2 and PRIMA PI resp. there was 7y PFS probability in LRG 76.1%, 71.3% and 72.6% resp., in IRG 63.7%, 61.1% and 57.7% resp., in HRG 46.9%, 45.6% and 42.4% resp. (Fig 1A). OS probability at 7y according to FLIPI, FLIPI2 and PRIMA PI resp. was in LRG 90.8%, 90.8% and 88.2% resp., in IRG 87.0%, 82.7% and 89.2% resp. and in HRG 75.2%, 73.1% and 68.0% resp. OS probability at 7y was 51.9% for those with POD24 vs 91.9% (median 7.1 vs nr) for those without POD24 (HR 7.1, p <0.0001). We tested impact of HR vs LG and IG (pooled into one group) PRIMA PI characteristic on OS separately in those pts with and without POD24. Among POD24 pts There was trend (p<0.11) for shorter OS for HRG pts vs others with median 6.2y vs 9.1y (HR 1.5). More importantly among pts without POD24 there was significantly higher risk to die for HRG patients vs others, HR 2.6 (p<0.0001) with 7y OS 83.4% vs 93.0% (fig 1B)
Conclusion
PRIMA PI represents feasible prognostic index which works in real world practice. Worse outcome of HRG pts is not given only by higher proportion of POD24 pts, but HRG pts compared to the others have greater risk to die (2.5x) even if they are late progressors.
Supported by grant AZV 16-31092A and Progres Q28 UK.
Session topic: 20. Indolent Non-Hodgkin lymphoma – Clinical
Keyword(s): Follicular lymphoma, prognosis, Survival
Abstract: S101
Type: Oral Presentation
Presentation during EHA23: On Friday, June 15, 2018 from 11:45 - 12:00
Location: Room A1
Background
Follicular lymphoma (FL) patients (pts) have high long-term survival probability in majority of cases, however some subgroups especially early progressors and pts with transformation poor outcome. Prognostic indexes could partially help and recently presented PRIMA PI (Bachy ASH2017) is the first one based on population of immunochemotherapy treated pts (PRIMA study).
Aims
Validation of PRIMA PI in large cohort of real world treated pts and analysis of impact of different PRIMA PI risk groups on progression within 24 months since start of therapy (POD24).
Methods
This analysis was part of NiHiL project (GovTrial No: NCT03199066). NiHiL project is based on prospective collection and analysis of diagnostic, epidemiologic and therapeutic data of NHL patients. All patients signed the informed consent approved by EC. The eligibility criteria were: all consecutively pts with confirmed FL dg, with confirmation of essential data (clinical characteristic, therapy, follow-up) treated with immunochemotherapy. Progression free survival (PFS) and Overall survival (OS) were counted since the therapy initiation. Pearson's Chi-square Test was used for group comparison, log rank test for survival analysis.
Results
Altogether 1179 pts diagnosed 1999-2015 and treated with immunochemotherapy in 1st line 2000-2015 fulfilled eligibility criteria. The majority (893) had grade 1 or 2, followed by gr 3A (188) or without given grade (98). Median age was 59y (26-87), BM was involved in 50.4% cases, LDH was elevated in 42.1% cases and beta2microglobulin >3mg/l in 31.8% of pts. Low risk group (LRG) according to FLIPI, FLIPI2 and PRIMA PI resp. represent 20.5%, 35.5% and 39.0% pts resp., intermediate risk group (IRG) 31.3%, 25.6% and 29.2% pts resp., high risk group (HRG) 48.1%, 38.9% and 31.8% pts resp. All patients were treated with rituximab and majority of pts (76.3%) were treated with CHOP, CVP was used in 13.3% pts, bendamustine 2.8%, fludarabine 2.6% and the rest with other regimens according to centres policy (PACEBO, sequential protocol and others). ORR (Cheson 1999) was reached in 92.4% of pts, out of these 66.7% received rituximab maintenance. With the median follow-up 6.1y there was 7y PFS and OS probability 58.7% and 82.3%. According to FLIPI, FLIPI2 and PRIMA PI resp. there was 7y PFS probability in LRG 76.1%, 71.3% and 72.6% resp., in IRG 63.7%, 61.1% and 57.7% resp., in HRG 46.9%, 45.6% and 42.4% resp. (Fig 1A). OS probability at 7y according to FLIPI, FLIPI2 and PRIMA PI resp. was in LRG 90.8%, 90.8% and 88.2% resp., in IRG 87.0%, 82.7% and 89.2% resp. and in HRG 75.2%, 73.1% and 68.0% resp. OS probability at 7y was 51.9% for those with POD24 vs 91.9% (median 7.1 vs nr) for those without POD24 (HR 7.1, p <0.0001). We tested impact of HR vs LG and IG (pooled into one group) PRIMA PI characteristic on OS separately in those pts with and without POD24. Among POD24 pts There was trend (p<0.11) for shorter OS for HRG pts vs others with median 6.2y vs 9.1y (HR 1.5). More importantly among pts without POD24 there was significantly higher risk to die for HRG patients vs others, HR 2.6 (p<0.0001) with 7y OS 83.4% vs 93.0% (fig 1B)
Conclusion
PRIMA PI represents feasible prognostic index which works in real world practice. Worse outcome of HRG pts is not given only by higher proportion of POD24 pts, but HRG pts compared to the others have greater risk to die (2.5x) even if they are late progressors.
Supported by grant AZV 16-31092A and Progres Q28 UK.
Session topic: 20. Indolent Non-Hodgkin lymphoma – Clinical
Keyword(s): Follicular lymphoma, prognosis, Survival


