
Contributions
Abstract: PB2205
Type: Publication Only
Background
Antiphospholipid antibodies (APA) are a group of proteins directed against the phospholipids of cell membranes, such as cardiolipins or phospholipid binding proteins. APA presence provokes microvascular, arterial or venous thrombotic events indicating somehow the relationship between the immune system, the hemostatic system, and the inflammatory response. It has been suggested that their presence in a critically ill patient is related to thrombotic manifestations, organ dysfunction, and death.
Aims
The aim of this study was to evaluate the prevalence of antiphospholipid antibodies in critically ill patients with autoimmune diseases and the rate of organ involvement.
Methods
Retrospective and descriptive study of patients admitted to the intensive care unit of Hospital Universidad de la Samaritana between 2008 and 2016, in Bogotá, Colombia.
Results
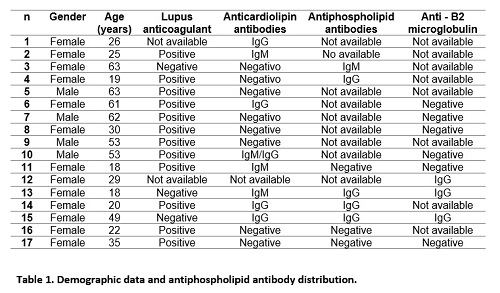
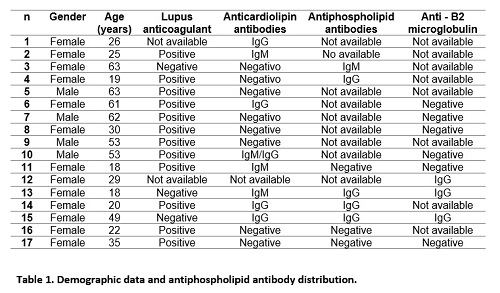
A total of 79 patients were found to have systemic lupus erythematosus (SLE), antiphospholipid syndrome and vasculitis. 17 patients (22%) were positive for antiphospholipid antibodies. Of these, 76% were women and mean age was 38 years (18-63 years). APA profiles showed positivity with this distribution: one positive antibody, n=9 patients (53%) (lupus anticoagulant antibody being the most common), two positive antibodies in n=4 patients (23%) and three positive antibodies in n=4 patients.
Conclusion
Session topic: 34. Thrombosis and vascular biology
Keyword(s): Autoimmune disease, Antiphospholipid antibody
Abstract: PB2205
Type: Publication Only
Background
Antiphospholipid antibodies (APA) are a group of proteins directed against the phospholipids of cell membranes, such as cardiolipins or phospholipid binding proteins. APA presence provokes microvascular, arterial or venous thrombotic events indicating somehow the relationship between the immune system, the hemostatic system, and the inflammatory response. It has been suggested that their presence in a critically ill patient is related to thrombotic manifestations, organ dysfunction, and death.
Aims
The aim of this study was to evaluate the prevalence of antiphospholipid antibodies in critically ill patients with autoimmune diseases and the rate of organ involvement.
Methods
Retrospective and descriptive study of patients admitted to the intensive care unit of Hospital Universidad de la Samaritana between 2008 and 2016, in Bogotá, Colombia.
Results
A total of 79 patients were found to have systemic lupus erythematosus (SLE), antiphospholipid syndrome and vasculitis. 17 patients (22%) were positive for antiphospholipid antibodies. Of these, 76% were women and mean age was 38 years (18-63 years). APA profiles showed positivity with this distribution: one positive antibody, n=9 patients (53%) (lupus anticoagulant antibody being the most common), two positive antibodies in n=4 patients (23%) and three positive antibodies in n=4 patients.
Conclusion
Session topic: 34. Thrombosis and vascular biology
Keyword(s): Autoimmune disease, Antiphospholipid antibody


