
Contributions
Abstract: PB2199
Type: Publication Only
Background
With the improvement in availability of blood transfusion practices and progress in chelation therapy, there is an increasing population of thalassemic patients surviving into adulthood in developing countries. However, there is scarcity of clinical, biochemical and radiological data showing cardiac and hepatic iron assessment in these chronically transfused individuals.
Aims
- Cardiac and hepatic iron assessment in young adults with TDT
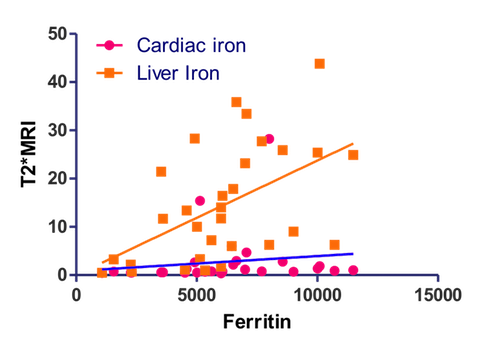
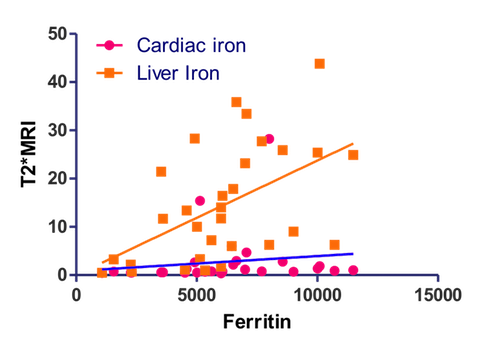
- Compare the ferritin level with T2* MRI finding
Methods
in this prospective observational study we analysed demographic details, clinical features and cardiac and liver iron assessment of young adults with (TDT) at recently established adult thalassemia clinic at PGIMER, Chandigarh. For cardiac and liver iron assessment serum ferritin, ECG, 2D Echo, MUGA scan, Liver function test, Fibroscan (if indicated) and T2* MRI of Liver and heart was done. All patients who were diagnosed in childhood and referred to adult haematology unit at age ≥18 years and had received more than 20 blood transfusions were included in the study.
Results
A total of 53 patients (n=53) were analysed. The mean age was 23 yrs. Majority of patients (56%) were male. The average age at diagnosis and at first transfusion was 7 months & 11months respectively. The average years of PRBC transfusion was 23 yrs. The average number of transfusion in last two years prior to registration was 24 PRBC units. The mean age at start of chelation was 10.0 yrs. Mean duration of chelation was 14 yrs. Majority (88%) had growth failure with mean height of 159.6 cm & mean weight of 51.5 kg respectively. Splenomegaly was present in 47% and hepatomegaly in 25 %patients. Twenty-eight percent have undergone splenectomy at an average age of 12.6 yrs. The mean of highest ferritin levels was 6131 ng/mL and the mean ferritin at the time of registration was 2919 ng/mL. LFT were deranged in 25% of patients. Evidence of cardiac dysfunction (ECG/MUGA) was present in 22% of patients. Iron overload in liver and heart as measured with T2* MRI was present in 56% & 28% respectively.
Conclusion
majority of patients registered in our clinic are living a healthy life. All of them were on iron chelation therapy and the dose was being adjusted as per the serum ferritin level. Amongst asymptomatic individuals with no evidence of cardiac or hepatic dysfunction, evaluation by T2*MRI picked up evidence of hepatic and cardiac iron overload. Therefore, its prudent to monitor patients with T2*MRI and accordingly escalate or de-escalate chelation therapy.
Session topic: 26. Thalassemias
Keyword(s): Thalassemia, MRI, iron chelation, Ferritin
Abstract: PB2199
Type: Publication Only
Background
With the improvement in availability of blood transfusion practices and progress in chelation therapy, there is an increasing population of thalassemic patients surviving into adulthood in developing countries. However, there is scarcity of clinical, biochemical and radiological data showing cardiac and hepatic iron assessment in these chronically transfused individuals.
Aims
- Cardiac and hepatic iron assessment in young adults with TDT
- Compare the ferritin level with T2* MRI finding
Methods
in this prospective observational study we analysed demographic details, clinical features and cardiac and liver iron assessment of young adults with (TDT) at recently established adult thalassemia clinic at PGIMER, Chandigarh. For cardiac and liver iron assessment serum ferritin, ECG, 2D Echo, MUGA scan, Liver function test, Fibroscan (if indicated) and T2* MRI of Liver and heart was done. All patients who were diagnosed in childhood and referred to adult haematology unit at age ≥18 years and had received more than 20 blood transfusions were included in the study.
Results
A total of 53 patients (n=53) were analysed. The mean age was 23 yrs. Majority of patients (56%) were male. The average age at diagnosis and at first transfusion was 7 months & 11months respectively. The average years of PRBC transfusion was 23 yrs. The average number of transfusion in last two years prior to registration was 24 PRBC units. The mean age at start of chelation was 10.0 yrs. Mean duration of chelation was 14 yrs. Majority (88%) had growth failure with mean height of 159.6 cm & mean weight of 51.5 kg respectively. Splenomegaly was present in 47% and hepatomegaly in 25 %patients. Twenty-eight percent have undergone splenectomy at an average age of 12.6 yrs. The mean of highest ferritin levels was 6131 ng/mL and the mean ferritin at the time of registration was 2919 ng/mL. LFT were deranged in 25% of patients. Evidence of cardiac dysfunction (ECG/MUGA) was present in 22% of patients. Iron overload in liver and heart as measured with T2* MRI was present in 56% & 28% respectively.
Conclusion
majority of patients registered in our clinic are living a healthy life. All of them were on iron chelation therapy and the dose was being adjusted as per the serum ferritin level. Amongst asymptomatic individuals with no evidence of cardiac or hepatic dysfunction, evaluation by T2*MRI picked up evidence of hepatic and cardiac iron overload. Therefore, its prudent to monitor patients with T2*MRI and accordingly escalate or de-escalate chelation therapy.
Session topic: 26. Thalassemias
Keyword(s): Thalassemia, MRI, iron chelation, Ferritin


