Abstract: PB2179
Type: Publication Only
Background
Allogenic hematopoietic stem cell transplantation (allo-HSCT) is an effective therapy for a variety of hematological malignancies. However, a lack of HLA-identical sibling donors or unrelated donors has restricted the application of allo-HSCT in hematological malignancies. Haploidentical HSCT (Haplo-HSCT) offers the benefits of rapid and nearly universal donor availability and, in the past decade, has been accepted worldwide as an alternative treatment for patients with hematological malignancies who do not have an HLA-identical sibling donor or who require urgent transplantation.
Aims
The purpose of this study was to investigate the incidence, causes and factors influencing overall and transplant-related mortality after Haplo-HSCT.
Methods
We analyzed all consecutive patients receiving Haplo-HSCT from family donors at our hospital from 2013 to 2016. The conditioning regimen used for the transplant was the Hopkins haplo protocol with high dose Cy (50 mg/kg on days 3 and 4) posttransplantation. We classified the patients before the Haplo-HSCT according to disease risk index (DRI), ECOG, Sorror score and EBMT risk score to evaluate the correlation between the physical state of the patients before the transplant and the survival (overall mortality (OM) and transplant-related mortality (TRM)). We used SPSS V.23 to calculate the cumulative Mortality incidence by the KM test and the Cox proportional hazards model.
Results
We performed 20 haplo-HSCT, 10 were males (1 was transplanted 3 times) and 8 were females mean age of 40 (range 16-64). Diagnosis: AML (10), ALL (1), EH (5), NHL (3), AM (1). Forty five percent of patients received the haplo-HSCT in remission, 50% with refractory disease and 5% of patients did not receive previous treatment.
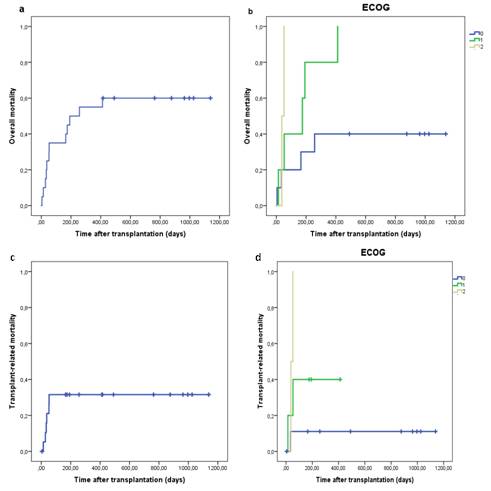
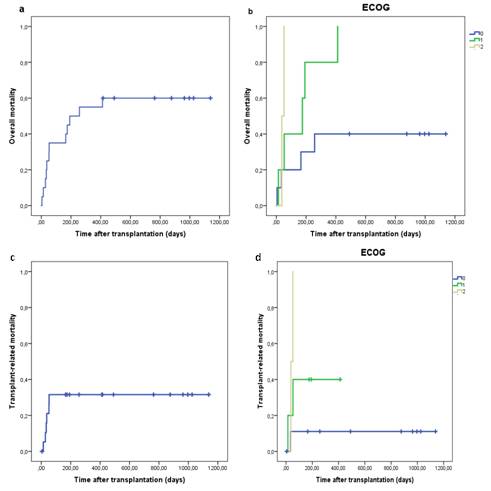
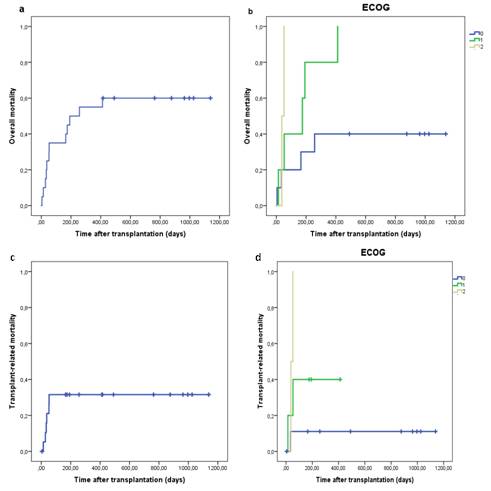
Of the 20 patients from our series, 12 died post transplant with an OM of 60%. The cumulative incidence (CI) of OM was 15% at 1 month (m), 35% at 3 m, 45% at 6 m, 55% at 1 year, and 40% at 2 and 3 years (Fig1a). When we analyzed the OM depending on the different physical status scores we found no statistically significant difference between OM from the different states of EBMT (p=0.356) and DRI (p=0.07), however we found a statistically significant difference for ECOG (p=0.028) (Fig1b) and Sorror (p=0.016). On a pairwise analysis of the OM we found no statistically signification for EBMT, and found a statistically significant difference between the patients with low-high DRI (p=0.01), intermediate-high DRI (p=0.01), ECOG 0-1 (p=0.046) and Sorror 0-5 (p=0.003). The multivariate analysis showed that ECOG 2 vs 0 (p=0.013, HR=46.59), Sorror 2-3 vs 0-1 (p=0.041, HR=19.55) and Sorror 4-5 vs 0-1 (p=0.005, HR=282.48) were significantly related with a higher incidence of OM. Five patients died of infection (41.67%), 3 of disease progression (25%), 1 of relapse (8.33%) and 3 of other causes (25%).
Six patients died of TRM (50%). The CI of TRM was 10.5% at 1 m and 31.6% at 3 m, 6 m, 1, 2 and 3 years (Fig1c). When we analyzed the TRM depending on the different physical status scores we only found a statistically significant difference between TRM incidence from the different states of ECOG (p=0.038) (Fig1d) and no statistically significant difference for EBMT (p=0.386), DRI (p=0.372) and Sorror (p=0.073). On the pairwise analysis we also found statistically significant differences between ECOG 1-2 (p=0.018) and EBMT 1-5 (p=0.046), for Sorror we found a marginal statistical signification between 0-1 (p=0.052), 0-2 (p=0.052) and 0-5 (p=0.052), for DRI we found no statistically significant difference. On the multivariate analysis we found no statistically significant correlation between TRM and the physical status scores.
Conclusion
Despite the fact that Sorror, EBMT and DRI scores are widely validated to establish the risk of patients undergoing HSCT, in our experience ECOG remains a useful score for assessing the risk of TRM on patients receiving Haplo-HSCT. We think further studies with a larger sample would be necessary to confirm our results.
Session topic: 22. Stem cell transplantation - Clinical