
Contributions
Abstract: PB2175
Type: Publication Only
Background
Although the Bruton tyrosine kinase (BTK) inhibitor ibrutinib significantly improves the prognosis of CLL patients (pts), allogeneic hematological stem cell transplantation (HCT) remains the only curative option for the underlying disease. Data on pre-transplant treatment of CLL with ibrutinib are very limited.
Aims
Here we present our experience of HCT in pts previously treated with ibrutinib.
Methods
11 CLL pts (median age at HCT 57 years [y], range 52-66 y) treated between 2014 and 2016 in our unit with non-myeloablative (nma) HCT after ibrutinib were included. Ibrutinib treatment lasted median 4.03 months (range 1 - 28). Conditioning regimen was Fludarabin 30 mg/m2 on day -4 to -2 followed by 2 Gy total body irradiation. Disease status at HCT was Binet B (n=3) or Binet C (n=8). Two pts had Richter’s transformation (RT) diagnosed before nma-HCT. Ten pts were in partial remission (PR) at nma-HCT (PR1 n=4; PR2 n=3; PR3 n=2, PR4 n=1) while one was in first relapse. Donors were human leukocyte antigen (HLA) matched related (n=3, MRD) or HLA-matched unrelated (n=8, MUD). Pts received median 3 lines of therapy (range 1-6) including ibrutinib before transplantation. Classical cytogenetic analysis and fluorescence in situ hybridization (FISH) was carried out for every pt. Five pts had a deletion (del)(17p13) and one a del(11q22.3).
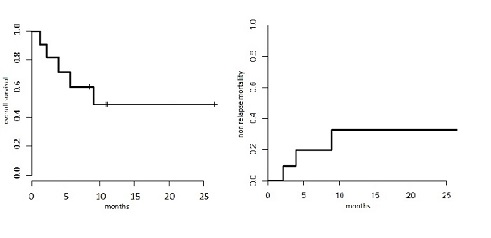
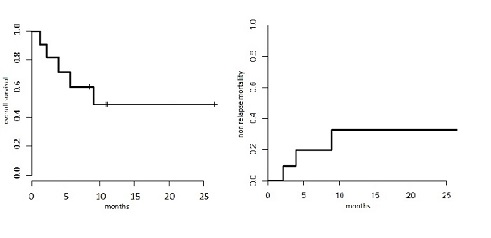
Results
Conclusion
The outcome in this small group is comparable to studies of CLL-pts undergoing nma-HCT without receiving ibrutinib upfront. Previous data from our unit (Hebenstreit et al., Leuk Lymphoma 2014) showed OS 51% and NRM 30% at 4y. Ibrutinib appears to be a feasible option in a transplantation setting, although further testing with larger numbers of patients and a longer follow up is required.
Session topic: 22. Stem cell transplantation - Clinical
Keyword(s): Chronic Lymphocytic Leukemia, Allogeneic hematopoietic stem cell transplant
Abstract: PB2175
Type: Publication Only
Background
Although the Bruton tyrosine kinase (BTK) inhibitor ibrutinib significantly improves the prognosis of CLL patients (pts), allogeneic hematological stem cell transplantation (HCT) remains the only curative option for the underlying disease. Data on pre-transplant treatment of CLL with ibrutinib are very limited.
Aims
Here we present our experience of HCT in pts previously treated with ibrutinib.
Methods
11 CLL pts (median age at HCT 57 years [y], range 52-66 y) treated between 2014 and 2016 in our unit with non-myeloablative (nma) HCT after ibrutinib were included. Ibrutinib treatment lasted median 4.03 months (range 1 - 28). Conditioning regimen was Fludarabin 30 mg/m2 on day -4 to -2 followed by 2 Gy total body irradiation. Disease status at HCT was Binet B (n=3) or Binet C (n=8). Two pts had Richter’s transformation (RT) diagnosed before nma-HCT. Ten pts were in partial remission (PR) at nma-HCT (PR1 n=4; PR2 n=3; PR3 n=2, PR4 n=1) while one was in first relapse. Donors were human leukocyte antigen (HLA) matched related (n=3, MRD) or HLA-matched unrelated (n=8, MUD). Pts received median 3 lines of therapy (range 1-6) including ibrutinib before transplantation. Classical cytogenetic analysis and fluorescence in situ hybridization (FISH) was carried out for every pt. Five pts had a deletion (del)(17p13) and one a del(11q22.3).
Results
Conclusion
The outcome in this small group is comparable to studies of CLL-pts undergoing nma-HCT without receiving ibrutinib upfront. Previous data from our unit (Hebenstreit et al., Leuk Lymphoma 2014) showed OS 51% and NRM 30% at 4y. Ibrutinib appears to be a feasible option in a transplantation setting, although further testing with larger numbers of patients and a longer follow up is required.
Session topic: 22. Stem cell transplantation - Clinical
Keyword(s): Chronic Lymphocytic Leukemia, Allogeneic hematopoietic stem cell transplant


