
Contributions
Abstract: PB2141
Type: Publication Only
Background
Aims
We aim to investigate if SDB could be a potential factor contributing to developmental problems in cognition in children and adolescent with SCD.
Methods
We have followed up children and adolescents in the Sleep Asthma cohort who underwent Polysomnography at two different time points (1) 2006-2009 and (2) 2011-2014 and compared the sleep data with subsequent neuropsychological assessment.
Results
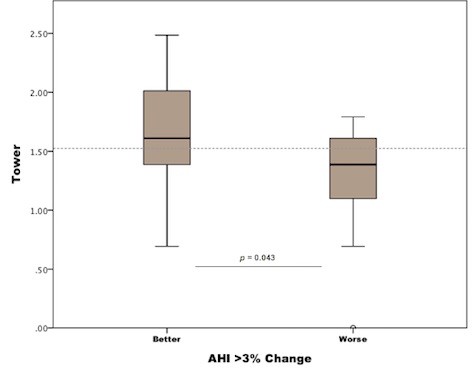
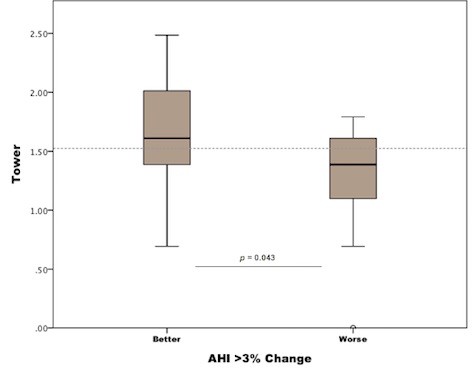
Worse performance was found for processing speed: PSI (p< 0.01) and general intelligence (p<0.05) compared to control siblings. SDB, measured as apnea and hypoxia index (i.e. AHI >3%: Apnoeas and hypopnoeas with more than ≥ 3% desaturation), was found to impact executive function, as measured with the Tower test, (p<0.05) and PSI (p<0.05). Mean oxygen saturation during total sleep time was significantly associated with lower PSI (p<0.05). Additionally, participants who showed a worsening of their SDB symptoms in their second sleep study had lower cognitive scores (i.e., executive function, p<0.05 and PSI, p<0.05).
Conclusion
Session topic: 25. Sickle cell disease
Keyword(s): Children, Treatment, Sickle cell patient, Development
Abstract: PB2141
Type: Publication Only
Background
Aims
We aim to investigate if SDB could be a potential factor contributing to developmental problems in cognition in children and adolescent with SCD.
Methods
We have followed up children and adolescents in the Sleep Asthma cohort who underwent Polysomnography at two different time points (1) 2006-2009 and (2) 2011-2014 and compared the sleep data with subsequent neuropsychological assessment.
Results
Worse performance was found for processing speed: PSI (p< 0.01) and general intelligence (p<0.05) compared to control siblings. SDB, measured as apnea and hypoxia index (i.e. AHI >3%: Apnoeas and hypopnoeas with more than ≥ 3% desaturation), was found to impact executive function, as measured with the Tower test, (p<0.05) and PSI (p<0.05). Mean oxygen saturation during total sleep time was significantly associated with lower PSI (p<0.05). Additionally, participants who showed a worsening of their SDB symptoms in their second sleep study had lower cognitive scores (i.e., executive function, p<0.05 and PSI, p<0.05).
Conclusion
Session topic: 25. Sickle cell disease
Keyword(s): Children, Treatment, Sickle cell patient, Development


