NOVEL TECHNIQUES FOR MONITORING GALNZMANN THROMBASTENIA PATIENT UNDERGOING SURGICAL INTERVENTIONS.
(Abstract release date: 05/18/17)
EHA Library. Barg A. 05/18/17; 182823; PB2109

Dr. Assaf Barg
Contributions
Contributions
Abstract
Abstract: PB2109
Type: Publication Only
Background
Glanzmann thrombasthenia (GT) patients undergoing surgical procedures are often treated by platelet transfusion. However many GT patients who have been previously exposed to platelets may form antibodies either against the missing αIIbβ3 antigen or directed against MHC-class molecules thus hampering the efficacy of care. Due to the rarity of disease there is paucity of data regarding platelet transfusion protocols during the perioperative period. We herein describe our experience with monitoring the proportion of donor platelets following transfusion, and their contribution to whole blood clot formation.
Aims
To describe the use of flow cytometry (FC) analysis in order to detect donor transfused platelets in A GT patient undergoing a minor surgical procedure and to assess the correlation between FC analysis and the results of Rotational thromboelastography(ROTEM).
Methods
A nine year old female patient with GT underwent teeth extraction. The Patient received platelet transfusion around the procedure. Complete blood counts, ROTEM, FC to detect the number of donor platelets and their ADP dependent activation, were sampled and followed till 7 days post teeth extraction.
Results
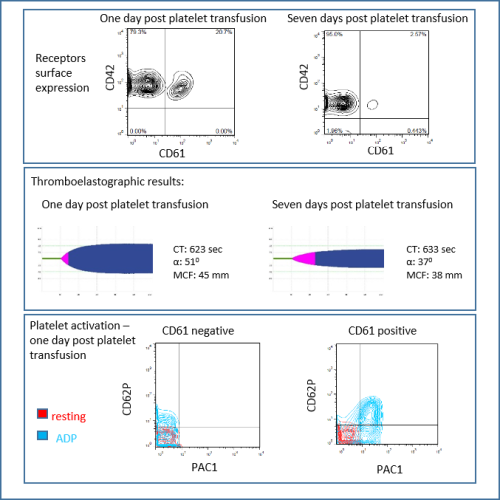
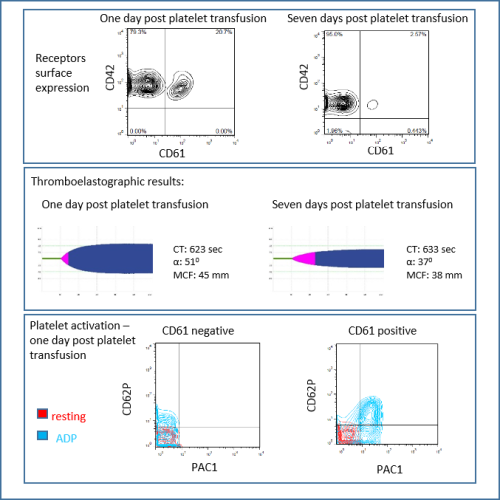
Prior to teeth extraction upon injection of local anesthetics patient developed a buccal hematoma probably owing to local blood vessel penetration. The patient did not experience any post extraction bleeding. Hematoma was absorbed within several days. Post transfusion platelets FC demonstrated 20.6%% donor platelets equivalent to 55,620 donor platelets. Platelets activation was determined following ADP addition by examination CD62 antigen expression. Seven days post platelet transfusion FC demonstrated 2.6% equivalent to 8,658 donor plantlets. The decline in the number of active platelets was associated with a reduced clot firmness (MCF) and lower α-angle as assessed by ROTEM [Figure 1].
Conclusion
Clinical decision making in patients with GT may be aided by application of novel techniques, evaluating the number of active donor platelets and actual clot formation. This data may help making more knowledgeable decisions as for the need for further platelet transfusion or for the need for rFVIIa. Thus leading to improved monitoring and better patients' care.
Session topic: 32. Platelets disorders
Keyword(s): transfusion, Surgery, Glanzmann, flow cytometry
Abstract: PB2109
Type: Publication Only
Background
Glanzmann thrombasthenia (GT) patients undergoing surgical procedures are often treated by platelet transfusion. However many GT patients who have been previously exposed to platelets may form antibodies either against the missing αIIbβ3 antigen or directed against MHC-class molecules thus hampering the efficacy of care. Due to the rarity of disease there is paucity of data regarding platelet transfusion protocols during the perioperative period. We herein describe our experience with monitoring the proportion of donor platelets following transfusion, and their contribution to whole blood clot formation.
Aims
To describe the use of flow cytometry (FC) analysis in order to detect donor transfused platelets in A GT patient undergoing a minor surgical procedure and to assess the correlation between FC analysis and the results of Rotational thromboelastography(ROTEM).
Methods
A nine year old female patient with GT underwent teeth extraction. The Patient received platelet transfusion around the procedure. Complete blood counts, ROTEM, FC to detect the number of donor platelets and their ADP dependent activation, were sampled and followed till 7 days post teeth extraction.
Results
Prior to teeth extraction upon injection of local anesthetics patient developed a buccal hematoma probably owing to local blood vessel penetration. The patient did not experience any post extraction bleeding. Hematoma was absorbed within several days. Post transfusion platelets FC demonstrated 20.6%% donor platelets equivalent to 55,620 donor platelets. Platelets activation was determined following ADP addition by examination CD62 antigen expression. Seven days post platelet transfusion FC demonstrated 2.6% equivalent to 8,658 donor plantlets. The decline in the number of active platelets was associated with a reduced clot firmness (MCF) and lower α-angle as assessed by ROTEM [Figure 1].
Conclusion
Clinical decision making in patients with GT may be aided by application of novel techniques, evaluating the number of active donor platelets and actual clot formation. This data may help making more knowledgeable decisions as for the need for further platelet transfusion or for the need for rFVIIa. Thus leading to improved monitoring and better patients' care.
Session topic: 32. Platelets disorders
Keyword(s): transfusion, Surgery, Glanzmann, flow cytometry
{{ help_message }}
{{filter}}


