
Contributions
Abstract: PB2100
Type: Publication Only
Background
Sepsis is a relatively common diagnosis in the neonatal period. Apart from blood cultures which are the gold standard, C-reactive protein (CRP), total white blood cell count (WBC) and the ratio of immature to mature neutrophils (I:T) are considered to be useful markers of sepsis in the neonatal period. There are a few studies that show that mean platelet volume (MPV) is elevated in infectious disease processes.
Aims
The aim of this study was to investigate whether mean platelet volume is increased in neonates with sepsis.
Methods
Only term neonates were included in the study. Exclusion criteria included: (a) Any neonate born with a genetic defect, (b) Any neonate with suspected immunodeficiency, (c) Any neonate requiring surgery in the post-natal period, (d) Neonates admitted to NICU for hyperbilirubinemia, (e) Neonates requiring extensive resuscitation at birth resulting in documented Hypoxic Ischemic Encephalopathy or requiring transfer to a Regional Perinatal Center.
Results
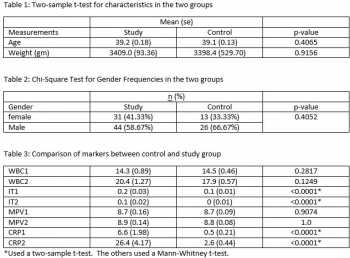
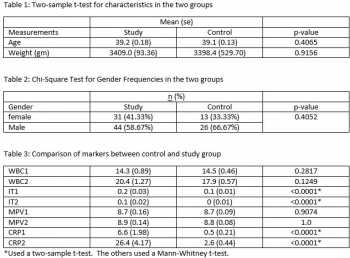
There was no statistically significant difference in the mean platelet volume between the study group and the control group (p value 0.9 in the first 24 hours and p value of 1 in the 24-48 hour sample). There was however, a statistically significant difference between immature to total neutrophil count and C-reactive protein on both samples (p value <0.0001).
Conclusion
Session topic: 32. Platelets disorders
Abstract: PB2100
Type: Publication Only
Background
Sepsis is a relatively common diagnosis in the neonatal period. Apart from blood cultures which are the gold standard, C-reactive protein (CRP), total white blood cell count (WBC) and the ratio of immature to mature neutrophils (I:T) are considered to be useful markers of sepsis in the neonatal period. There are a few studies that show that mean platelet volume (MPV) is elevated in infectious disease processes.
Aims
The aim of this study was to investigate whether mean platelet volume is increased in neonates with sepsis.
Methods
Only term neonates were included in the study. Exclusion criteria included: (a) Any neonate born with a genetic defect, (b) Any neonate with suspected immunodeficiency, (c) Any neonate requiring surgery in the post-natal period, (d) Neonates admitted to NICU for hyperbilirubinemia, (e) Neonates requiring extensive resuscitation at birth resulting in documented Hypoxic Ischemic Encephalopathy or requiring transfer to a Regional Perinatal Center.
Results
There was no statistically significant difference in the mean platelet volume between the study group and the control group (p value 0.9 in the first 24 hours and p value of 1 in the 24-48 hour sample). There was however, a statistically significant difference between immature to total neutrophil count and C-reactive protein on both samples (p value <0.0001).
Conclusion
Session topic: 32. Platelets disorders


