
Contributions
Abstract: PB2084
Type: Publication Only
Background
Thrombotic microangiopathy (TMA) is a heterogeneous group of disease that has a fatal pattern of endothelial damage. TMA can be found in association with diverse clinical conditions such as carcinoma metastasis, malignant hypertension, infections, and TTP (thrombotic thrombocytopenic purpura). TTP is a rare, life-threatening multisystem disease, characterized by microangiopathic hemolytic anemia, thrombocytopenia, fever, renal dysfunction, and neurological disorders.
Aims
The purpose of this study is to evaluate the etiology associated with TMA.
Methods
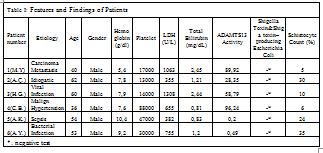
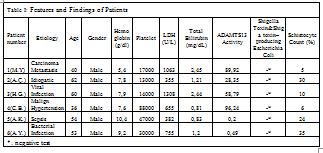
All of the six TMA patients who were newly admitted to our clinic in two months period were enrolled in this study. Effectiveness, response, adverse effects and safety of plasmapheresis were evaluated using laboratory and clinical findings. (See Table I)
Results
First patient presented with cachexia, thrombocytopenia, and TMA. He did not respond to plasmapheresis and corticosteroid treatment. We diagnosed carcinoma metastasis and liver metastasis, respectively, through bone marrow biopsy and PET(positron emission tomography). We thusly ascertained that TMA was due to carcinoma unknown primary. The second patient presented with general neurological findings like Guillain-Barre Syndrome and paraplegia with renal failure, thrombocytopenia, and TMA. After PLEX and corticosteroid treatment, laboratory and neurological clinical recovery were observed after one month. The third patient had chronic obstructive pulmonary disease and pneumonia in anamnesis. who presented with anemia, thrombocytopenia, fever and pneumonia findings. We conducted PLEX therapy. On the 8th day of PLEX, the patient had anaphylaxis, we performed cardio pulmonary resuscitation. The fourth patient presented with acute renal failure with malign hypertension. We performed hemodialysis together with PLEX treatment. Because his diagnosis was acute renal failure, malign hypertension, and TMA. The fifth patient presented with epistaxis and sepsis. He had chronic TTP diagnosis from two years ago. We diagnosed the patient as relapse TTP. Early treatment against infection and PLEX increased his platelet counts as early as the second day of treatment. The sixth patient presented with a fever that had been going on for five days. We treated the patient with PLEX together with the corticosteroid. Because his ADAMTS13 level was very low and he had 35% schistocytes.
Conclusion
We diagnosed our first patient with carcinoma unknown primary, who did not respond to PLEX and corticosteroid treatment. The results we received for that patient indicate that PLEX with corticosteroid treatment alone, remain ineffective in cancer-related TMA patients. Etiology of our second patients TMA was idiopathic. His clinical and laboratory findings improved rapidly in response to PLEX and pulse corticosteroid treatment. One viral infection induced TMA patient had anaphylactic reaction receiving his 8th PLEX. Allergic reactions should always be kept in mind when administering PLEX. One patient with TMA and malign hypertension-induced renal failure was successfully treated with PLEX, hemodialysis and antihypertensive treatment. We successfully treated our bacterial infection and sepsis-induced TTP patients with PLEX and antibiotic administration. In second TMA patient, we coupled PLEX with high dosage corticosteroid treatment even though he had an infection. For he had high schistocyte count and atypical neurological findings.ADAMTS 13 activity may only be a guide for diagnosis of TTP, but it is unreliable for a definitive one. In conclusion, diagnosis of TTP and other TMAs is difficult. Etiology, clinical features, laboratory findings should all be taken into account when diagnosing TMA. While it is established that ADAM TS13 deficiency is the major cause in acquired TTP, finding the etiology of other TMAs is determinant for a successful treatment of the latter.
Session topic: 31. Other Non-malignant hematopoietic disorders
Keyword(s): Thrombotic thrombocytopenic purpura (TTP), Thrombotic microangiopathy, ADAMTS13
Abstract: PB2084
Type: Publication Only
Background
Thrombotic microangiopathy (TMA) is a heterogeneous group of disease that has a fatal pattern of endothelial damage. TMA can be found in association with diverse clinical conditions such as carcinoma metastasis, malignant hypertension, infections, and TTP (thrombotic thrombocytopenic purpura). TTP is a rare, life-threatening multisystem disease, characterized by microangiopathic hemolytic anemia, thrombocytopenia, fever, renal dysfunction, and neurological disorders.
Aims
The purpose of this study is to evaluate the etiology associated with TMA.
Methods
All of the six TMA patients who were newly admitted to our clinic in two months period were enrolled in this study. Effectiveness, response, adverse effects and safety of plasmapheresis were evaluated using laboratory and clinical findings. (See Table I)
Results
First patient presented with cachexia, thrombocytopenia, and TMA. He did not respond to plasmapheresis and corticosteroid treatment. We diagnosed carcinoma metastasis and liver metastasis, respectively, through bone marrow biopsy and PET(positron emission tomography). We thusly ascertained that TMA was due to carcinoma unknown primary. The second patient presented with general neurological findings like Guillain-Barre Syndrome and paraplegia with renal failure, thrombocytopenia, and TMA. After PLEX and corticosteroid treatment, laboratory and neurological clinical recovery were observed after one month. The third patient had chronic obstructive pulmonary disease and pneumonia in anamnesis. who presented with anemia, thrombocytopenia, fever and pneumonia findings. We conducted PLEX therapy. On the 8th day of PLEX, the patient had anaphylaxis, we performed cardio pulmonary resuscitation. The fourth patient presented with acute renal failure with malign hypertension. We performed hemodialysis together with PLEX treatment. Because his diagnosis was acute renal failure, malign hypertension, and TMA. The fifth patient presented with epistaxis and sepsis. He had chronic TTP diagnosis from two years ago. We diagnosed the patient as relapse TTP. Early treatment against infection and PLEX increased his platelet counts as early as the second day of treatment. The sixth patient presented with a fever that had been going on for five days. We treated the patient with PLEX together with the corticosteroid. Because his ADAMTS13 level was very low and he had 35% schistocytes.
Conclusion
We diagnosed our first patient with carcinoma unknown primary, who did not respond to PLEX and corticosteroid treatment. The results we received for that patient indicate that PLEX with corticosteroid treatment alone, remain ineffective in cancer-related TMA patients. Etiology of our second patients TMA was idiopathic. His clinical and laboratory findings improved rapidly in response to PLEX and pulse corticosteroid treatment. One viral infection induced TMA patient had anaphylactic reaction receiving his 8th PLEX. Allergic reactions should always be kept in mind when administering PLEX. One patient with TMA and malign hypertension-induced renal failure was successfully treated with PLEX, hemodialysis and antihypertensive treatment. We successfully treated our bacterial infection and sepsis-induced TTP patients with PLEX and antibiotic administration. In second TMA patient, we coupled PLEX with high dosage corticosteroid treatment even though he had an infection. For he had high schistocyte count and atypical neurological findings.ADAMTS 13 activity may only be a guide for diagnosis of TTP, but it is unreliable for a definitive one. In conclusion, diagnosis of TTP and other TMAs is difficult. Etiology, clinical features, laboratory findings should all be taken into account when diagnosing TMA. While it is established that ADAM TS13 deficiency is the major cause in acquired TTP, finding the etiology of other TMAs is determinant for a successful treatment of the latter.
Session topic: 31. Other Non-malignant hematopoietic disorders
Keyword(s): Thrombotic thrombocytopenic purpura (TTP), Thrombotic microangiopathy, ADAMTS13


