
Contributions
Abstract: PB2052
Type: Publication Only
Background
Aims
To study the impact of driver gene mutations: Janus kinase 2 (JAK2), calreticulin (CALR) and myeloproliferative leukemia virus oncogene (MPL) on disease burden and correlating mutational status with symptom severity calculated by MPN10 score, degree of bone marrow (BM) fibrosis, clinical characteristics and survival in MPNs patients.
Methods
Results
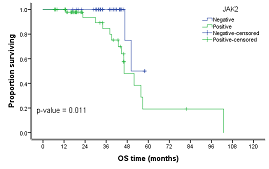
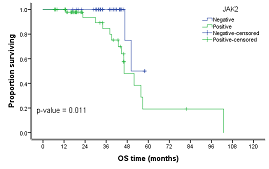
93 MPNs patients (48 males and 45 females): 18 polycythemia vera (PV), 41 essential thrombocythemia (ET), 24 primary myelofibrosis (PMF), 10 Post-ET/PV-myelofibrosis (post-ET/PV-MF) were included. Median age at diagnosis was 55 years (17-75) and was lower in ET than PV and PMF patients; 44 (19-75) years vs. 56 (34-70) years and 56 (20-75) years, respectively (p<0.001). JAK2 mutation was positive 53/93 (57%); 16 (90%) PV patients, 14 (34%) ET patients, 15 (62%) PMF patients, 8(80%) post-ET/PV-MF patients (p<0.001). CALR mutation was positive in 14/93 (15%); 10 (24%) ET patients, 4 (17%) PMF patients, zero (0%) Post-ET/PV-MF patients (p=0.050). MPL mutation was positive in 3/93 (3%); 2 (5%) ET patients, 1(4%) PMF patients, zero (0%) Post ET/PV-MF patients. 23/93 (25%) patients were triple negative; 15 ET, 2 PV, 4 PMF and 2 post ET-MF. Median MPN10 score was 21 (4-45) in ET versus 37.5 (25-56) in PV, 54 (15-80) in PMF and 59 (45-75) in Post-ET/PV-MF (p<0.001). From 39 patients with BM fibrosis, 6 (15%) were triple negative vs. 33 (85%) mutant patients (p=0.007). Among 52 patients with splenomegaly; 7 (13.5%) patients were triple negative vs. 45 (87%) patients with a positive mutational status (p<0.001). Median MPN10 score was 48 (5-76) in JAK2 positive patients vs. 25 (4-80) in JAK2 negative (p<0.001) and was 22.5 (4-65) in CALR mutants vs. 35 (5-80) in CALR negative (p<0.050). Median MPN10 score was 21 (10-48) in triple negative patients vs. 40 (4-80) in MPNs JAK2/CALR/MPL mutants (p<0.001).After a median follow-up period of 36 months (6.6-102), progression free survival (PFS) and overall survival (OS) of the whole cohort was 85% and 95%, respectively. PFS of JAK2 positive vs negative patients was 62% vs 100% (p<0.001). PFS of CALR positive vs negative patients was 100% vs 78% (p=0.067). PFS of triple negative vs mutant patients was 100% vs 75% (p=0.004). OS of JAK2 positive vs negative patients was 85% vs 100% (p=0.011). OS of CALR positive vs negative patients was 100% vs 92% (p=0.197). OS of triple negative vs mutant patients was 100% vs 90% (p=0.015).
Conclusion
MPN10 score is directly affected by JAK2 and CALR positivity and can be used as a major predictor of survival in MPNs patients. Triple negative ET patients in our cohort have significantly lower MPN10 score, show lower incidence of BM fibrosis and splenomegaly which may indicate a more indolent disease course.
Session topic: 16. Myeloproliferative neoplasms - Clinical
Keyword(s): Survival, Myeloproliferative disorder
Abstract: PB2052
Type: Publication Only
Background
Aims
To study the impact of driver gene mutations: Janus kinase 2 (JAK2), calreticulin (CALR) and myeloproliferative leukemia virus oncogene (MPL) on disease burden and correlating mutational status with symptom severity calculated by MPN10 score, degree of bone marrow (BM) fibrosis, clinical characteristics and survival in MPNs patients.
Methods
Results
93 MPNs patients (48 males and 45 females): 18 polycythemia vera (PV), 41 essential thrombocythemia (ET), 24 primary myelofibrosis (PMF), 10 Post-ET/PV-myelofibrosis (post-ET/PV-MF) were included. Median age at diagnosis was 55 years (17-75) and was lower in ET than PV and PMF patients; 44 (19-75) years vs. 56 (34-70) years and 56 (20-75) years, respectively (p<0.001). JAK2 mutation was positive 53/93 (57%); 16 (90%) PV patients, 14 (34%) ET patients, 15 (62%) PMF patients, 8(80%) post-ET/PV-MF patients (p<0.001). CALR mutation was positive in 14/93 (15%); 10 (24%) ET patients, 4 (17%) PMF patients, zero (0%) Post-ET/PV-MF patients (p=0.050). MPL mutation was positive in 3/93 (3%); 2 (5%) ET patients, 1(4%) PMF patients, zero (0%) Post ET/PV-MF patients. 23/93 (25%) patients were triple negative; 15 ET, 2 PV, 4 PMF and 2 post ET-MF. Median MPN10 score was 21 (4-45) in ET versus 37.5 (25-56) in PV, 54 (15-80) in PMF and 59 (45-75) in Post-ET/PV-MF (p<0.001). From 39 patients with BM fibrosis, 6 (15%) were triple negative vs. 33 (85%) mutant patients (p=0.007). Among 52 patients with splenomegaly; 7 (13.5%) patients were triple negative vs. 45 (87%) patients with a positive mutational status (p<0.001). Median MPN10 score was 48 (5-76) in JAK2 positive patients vs. 25 (4-80) in JAK2 negative (p<0.001) and was 22.5 (4-65) in CALR mutants vs. 35 (5-80) in CALR negative (p<0.050). Median MPN10 score was 21 (10-48) in triple negative patients vs. 40 (4-80) in MPNs JAK2/CALR/MPL mutants (p<0.001).After a median follow-up period of 36 months (6.6-102), progression free survival (PFS) and overall survival (OS) of the whole cohort was 85% and 95%, respectively. PFS of JAK2 positive vs negative patients was 62% vs 100% (p<0.001). PFS of CALR positive vs negative patients was 100% vs 78% (p=0.067). PFS of triple negative vs mutant patients was 100% vs 75% (p=0.004). OS of JAK2 positive vs negative patients was 85% vs 100% (p=0.011). OS of CALR positive vs negative patients was 100% vs 92% (p=0.197). OS of triple negative vs mutant patients was 100% vs 90% (p=0.015).
Conclusion
MPN10 score is directly affected by JAK2 and CALR positivity and can be used as a major predictor of survival in MPNs patients. Triple negative ET patients in our cohort have significantly lower MPN10 score, show lower incidence of BM fibrosis and splenomegaly which may indicate a more indolent disease course.
Session topic: 16. Myeloproliferative neoplasms - Clinical
Keyword(s): Survival, Myeloproliferative disorder


