
Contributions
Abstract: PB2034
Type: Publication Only
Background
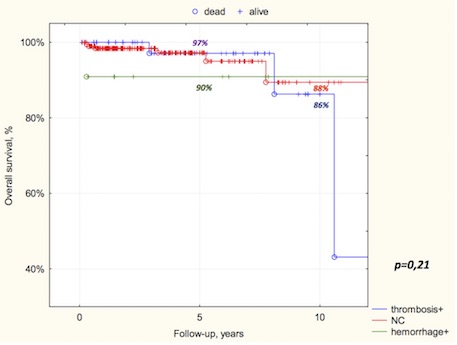
Thrombosis and hemorrhage are the main category of complications, that affects the overall survival (OS), quality of life and therapy option choice in essential thrombocythemia (ET). Molecular marker presence (JAK2V617F, MPL, CALR) or its absence (triple-negative status (TN)) in ET supposed to impact on the clinical course, thrombosis rate and ET prognosis.
Aims
Methods
Results
Conclusion
Leukocytosis >11x109/l and thrombocytosis >1000x109/l cannot be assessed as independent thrombosis risk factors in ET. JAK2V617F mutation was associated with increased risk of thrombotic complications in ET. CALR mutations were correlated with lower thrombosis risk and better OS rate, comparing to JAK2+ and TN status despite the fact of CALR+ patients had higher platelets level. Along with common thrombosis risk factors (age >60 and cardiovascular risk factors) mutational status may help to identify ET course and to optimize individual therapy option choice.
Session topic: 16. Myeloproliferative neoplasms - Clinical
Keyword(s): Mutation status, Essential Thrombocytemia
Abstract: PB2034
Type: Publication Only
Background
Thrombosis and hemorrhage are the main category of complications, that affects the overall survival (OS), quality of life and therapy option choice in essential thrombocythemia (ET). Molecular marker presence (JAK2V617F, MPL, CALR) or its absence (triple-negative status (TN)) in ET supposed to impact on the clinical course, thrombosis rate and ET prognosis.
Aims
Methods
Results
Conclusion
Leukocytosis >11x109/l and thrombocytosis >1000x109/l cannot be assessed as independent thrombosis risk factors in ET. JAK2V617F mutation was associated with increased risk of thrombotic complications in ET. CALR mutations were correlated with lower thrombosis risk and better OS rate, comparing to JAK2+ and TN status despite the fact of CALR+ patients had higher platelets level. Along with common thrombosis risk factors (age >60 and cardiovascular risk factors) mutational status may help to identify ET course and to optimize individual therapy option choice.
Session topic: 16. Myeloproliferative neoplasms - Clinical
Keyword(s): Mutation status, Essential Thrombocytemia


