
Contributions
Abstract: PB2004
Type: Publication Only
Background
Paraproteinemic neuropathy (PPN) refers to a disorder of the peripheral nervous system associated with a monoclonal gammopathy (MG). It is known that about 10% of idiopathic peripheral neuropathies are of this type. Unfortunately, PPN is often underdiagnosed or confused with chronic inflammatory demyelinating polyneuropathy (CIDP), subsequently leading to inappropriate management. Since progression of neuropathy is associated with possible malignant conversion of underlying monoclonal gammopathy, it is important to recognize underlying hematological conditions.
Aims
We aimed to determine whether the clinical characteristics and course differed in patients with PPN compared to those with CIDP in order to identify factors useful for differential diagnosis.
Methods
This study was carried out at Seoul National University Hospital, which is a tertiary academic center. During the period between January 2005 and December 2016, patients with 1) monoclonal gammopathy of undetermined significance (MGUS), and 2 CIDP were identified. Those with previous history of cancer or autoimmune disease requiring treatment with immunodulatory agents were excluded from analyses. In the end, a total of 18 MGUS patients and 34 CIDP patients, with complete set of data including clinical physical examinations, electrodiagnostic studies, and laboratory test results, were enrolled.
Results
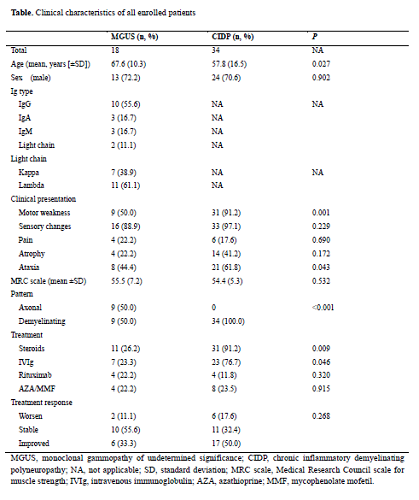
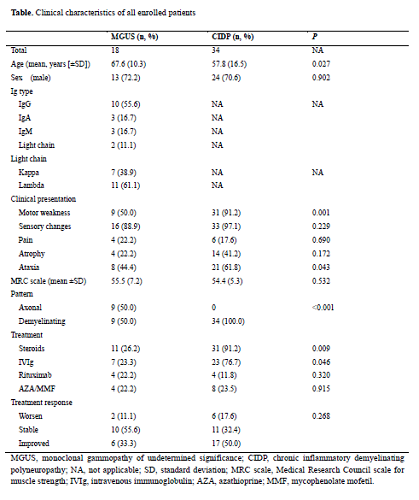
In both groups, males were predominant. IgG MG was most common (55.6%) in our cohort. PPN appeared to be mainly sensory regardless of heavy chain or light chain. Compared to PPN patients, CIDP patients were associated with motor symptoms manifesting as motor weakness (50.0% versus 91.2%, P=0.001) and ataxia (44.4% versus 61.8%, P=0.043) (Table). There were equal number of axonal type neuropathy and demyelinating type neuropathy in patients with PPN, and there were no differences in type of neuropathy between various immunoglobulin subclasses. However, demyelinating type PPN was associated with more severe clinical presentations, including more dysethesia, pain and sensory symptoms. During median follow-up of 49 months, 2 PPN patients developed overt hematologic malignancies: 1 case of Waldenstrom macroglobulinemia and 1 case of AL amyloidosis. Both of them showed malignant transformation within 8 months of neuropathy development, and were associated with worsening neuropathic symptom at the diagnosis of hematologic malignancy. There were no differences between the two groups with regards to overall survival.
Conclusion
Although both PPN and CIDP patients suffer from sensory symptoms, CIDP patients were more often associated with superimposed motor symptoms. Among PPN patients, demyelinating type neuropathy seems to be associated with more severe clinical presentations. Worsening of neuropathic symptoms in PPN patients warrants a high level of suspicion of malignant transformation of underlying disease.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Monoclonal antibody
Abstract: PB2004
Type: Publication Only
Background
Paraproteinemic neuropathy (PPN) refers to a disorder of the peripheral nervous system associated with a monoclonal gammopathy (MG). It is known that about 10% of idiopathic peripheral neuropathies are of this type. Unfortunately, PPN is often underdiagnosed or confused with chronic inflammatory demyelinating polyneuropathy (CIDP), subsequently leading to inappropriate management. Since progression of neuropathy is associated with possible malignant conversion of underlying monoclonal gammopathy, it is important to recognize underlying hematological conditions.
Aims
We aimed to determine whether the clinical characteristics and course differed in patients with PPN compared to those with CIDP in order to identify factors useful for differential diagnosis.
Methods
This study was carried out at Seoul National University Hospital, which is a tertiary academic center. During the period between January 2005 and December 2016, patients with 1) monoclonal gammopathy of undetermined significance (MGUS), and 2 CIDP were identified. Those with previous history of cancer or autoimmune disease requiring treatment with immunodulatory agents were excluded from analyses. In the end, a total of 18 MGUS patients and 34 CIDP patients, with complete set of data including clinical physical examinations, electrodiagnostic studies, and laboratory test results, were enrolled.
Results
In both groups, males were predominant. IgG MG was most common (55.6%) in our cohort. PPN appeared to be mainly sensory regardless of heavy chain or light chain. Compared to PPN patients, CIDP patients were associated with motor symptoms manifesting as motor weakness (50.0% versus 91.2%, P=0.001) and ataxia (44.4% versus 61.8%, P=0.043) (Table). There were equal number of axonal type neuropathy and demyelinating type neuropathy in patients with PPN, and there were no differences in type of neuropathy between various immunoglobulin subclasses. However, demyelinating type PPN was associated with more severe clinical presentations, including more dysethesia, pain and sensory symptoms. During median follow-up of 49 months, 2 PPN patients developed overt hematologic malignancies: 1 case of Waldenstrom macroglobulinemia and 1 case of AL amyloidosis. Both of them showed malignant transformation within 8 months of neuropathy development, and were associated with worsening neuropathic symptom at the diagnosis of hematologic malignancy. There were no differences between the two groups with regards to overall survival.
Conclusion
Although both PPN and CIDP patients suffer from sensory symptoms, CIDP patients were more often associated with superimposed motor symptoms. Among PPN patients, demyelinating type neuropathy seems to be associated with more severe clinical presentations. Worsening of neuropathic symptoms in PPN patients warrants a high level of suspicion of malignant transformation of underlying disease.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Monoclonal antibody


