
Contributions
Abstract: PB1990
Type: Publication Only
Background
Early mortality in the first 6 to 12 months from diagnosis is well recognized in newly diagnosed multiple myeloma (NDMM) patients, with rates in the real-world setting of around 20-30%
Aims
In a retrospective analysis of the causes of death performed by the end of 2012 we identify 2 different causes in the 2 consecutive periods analyzed. In the first period (1998-2006) the main cause was MM progression and in the second (2006-12) was secondary to serious infectious complications.
Methods
After this analysis several measures were taken to reduce this high early mortality:
1) To promote the ambulatory regime both in diagnosis and for the rapid assessment of complications to avoid or shorten income and to reduce these nosocomial-behaviour infection complications.
2) Early initiation of 'optimal' anti-myeloma treatment.
3) Get infectious prophylaxis in patients over 75 years and / or renal failure with Septrim ©.
Results
343 pac NDMM were treated between 1998 and 2015 (127 in the 1st period, 115 in the 2nd: 242 pts before 2013; and 101 in the 3rd period: 2013-15).
The median age at dx was 74 years (39-100). The number of patients died <6m was 77 years.
60 died before 6 months: 55 before 2013 (29 in the 1st period (22.8%) and 26 in the 2nd (22.6) and 5 after 2013 (5.0%).
Of these 60, 37 had a severe infectious complication.
The main cause of mortality before 2013 was infectious complications, (14 of 28 early death in the first period and 22 of 26 in the second).
Severe pneumococcal infections were infrequent (11%)
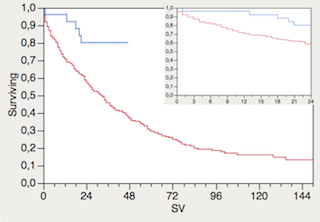
In the 3rd period, mortality <6m was reduced by 77% (22% vs 5%) (p.001); There was only 1 severe infection (G5) in this period (CMV reactivation, probably Pneumocystis pulmonary infection, E. Coli bacteriemia and a intestinal necrosis after an atrial fibrilation embolism) Figure 1 (upper corner)
Conclusion
Infectious complications and progression of MM have been the main cause of early mortality in patients with NDMM.
Identifying potential 'modifiable' variables and acting on them improves the short-term prognosis of patients with NDMM like: Supportive treatment to prevent infectious complications (avoid unnecesary hospitalization, antibiotical prophylaxis) and rapid access to optimal antiMM treatments.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Mortality
Abstract: PB1990
Type: Publication Only
Background
Early mortality in the first 6 to 12 months from diagnosis is well recognized in newly diagnosed multiple myeloma (NDMM) patients, with rates in the real-world setting of around 20-30%
Aims
In a retrospective analysis of the causes of death performed by the end of 2012 we identify 2 different causes in the 2 consecutive periods analyzed. In the first period (1998-2006) the main cause was MM progression and in the second (2006-12) was secondary to serious infectious complications.
Methods
After this analysis several measures were taken to reduce this high early mortality:
1) To promote the ambulatory regime both in diagnosis and for the rapid assessment of complications to avoid or shorten income and to reduce these nosocomial-behaviour infection complications.
2) Early initiation of 'optimal' anti-myeloma treatment.
3) Get infectious prophylaxis in patients over 75 years and / or renal failure with Septrim ©.
Results
343 pac NDMM were treated between 1998 and 2015 (127 in the 1st period, 115 in the 2nd: 242 pts before 2013; and 101 in the 3rd period: 2013-15).
The median age at dx was 74 years (39-100). The number of patients died <6m was 77 years.
60 died before 6 months: 55 before 2013 (29 in the 1st period (22.8%) and 26 in the 2nd (22.6) and 5 after 2013 (5.0%).
Of these 60, 37 had a severe infectious complication.
The main cause of mortality before 2013 was infectious complications, (14 of 28 early death in the first period and 22 of 26 in the second).
Severe pneumococcal infections were infrequent (11%)
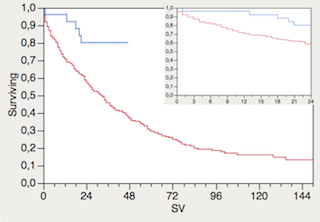
In the 3rd period, mortality <6m was reduced by 77% (22% vs 5%) (p.001); There was only 1 severe infection (G5) in this period (CMV reactivation, probably Pneumocystis pulmonary infection, E. Coli bacteriemia and a intestinal necrosis after an atrial fibrilation embolism) Figure 1 (upper corner)
Conclusion
Infectious complications and progression of MM have been the main cause of early mortality in patients with NDMM.
Identifying potential 'modifiable' variables and acting on them improves the short-term prognosis of patients with NDMM like: Supportive treatment to prevent infectious complications (avoid unnecesary hospitalization, antibiotical prophylaxis) and rapid access to optimal antiMM treatments.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Mortality


