EXTRAMEDULLARY MYELOMA IN THE “NOVEL AGENTS ERA”: OUTCOME, HETEROGENEITIES AND PECULIARITIES OF A COHORT OF 84 PATIENTS RETROSPECTIVELY ANALYSED IN A MONOCENTRIC EXPERIENCE
(Abstract release date: 05/18/17)
EHA Library. Torti L. 05/18/17; 182667; PB1953

Dr. Lorenza Torti
Contributions
Contributions
Abstract
Abstract: PB1953
Type: Publication Only
Background
Extramedullary disease is an uncommon manifestation in multiple myeloma(MM) and can either accompany newly diagnosed disease or develop with disease progression or relapse. Extramedullary myeloma(EMM)seems to have a different pathogenesis from its much more frequently encountered medullary counterpart, showing often a poor prognosis. EMM clinical situations are extraordinarily heterogeneous and their management is challenging.This includes organ or tissue involvement resulting from hematogenous-spread and/or bone involvement originating from different kind of bones.
Aims
We evaluated the impact of this disease features on patients’ outcome in the context of novel-agents.
Methods
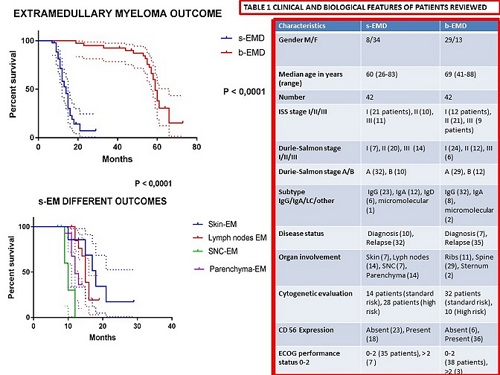
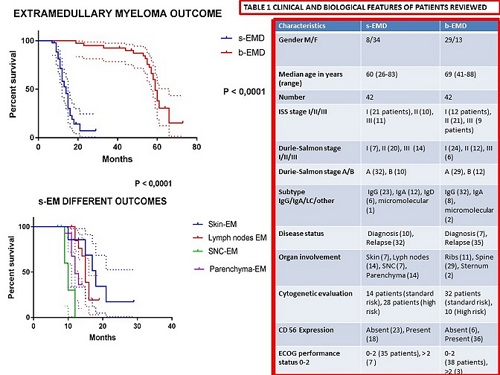
We reviewed 84 patients presenting EMM (median age 60, range 30-76)describing clinical and biological features(Table 1).Our aim was studying prognosis of bone-related extramedullary-disease (bEMD) and its relationship with soft-tissue related EMD (sEMD)in MM patients in our institution.
Results
42 bEMD and 42 sEMD patients treated at Our Department between 2007 and 2016 were included in this study. Of the first group 10 presented EMM at diagnosis and 32 at relapse as well as 7 and 35 respectevely of the second series.31 among sEMD were dead and 11 were alive, 20 of bEMD patients were dead and 22 were still alive. EM was diagnosed using imaging techiniques such as PET-CT (35%) or magnetic resonance MRI (65%).Biopsies were carried out only if the lesion was accessible (62%). The treatment was heterogeneous and all patients had receveid either thalidomide or bortezomib in the first-line of therapy. We showed that sEMD cohort has a significantly poorer survival compared to bEMD patients (median OS from diagnosis of EMD of 13 versus 58 months, P<0001). Finally lung, liver (parenchyma-EM)and SNC involvement among sEMD patients has shown a poorer outcome when compared to skin and lymph nodes masses respectively median OS of 12 and 10 months versus 18 and 15 months P <0001). Conversely among bEMD group there wasn’t a significant advantage of outcome regarding the different bones involved. Kaplan-Meier estimates were used for survival analysis and differences between survival-times in patient subgroups were tested using the log-rank test(Figure 1).Interestingly extramedullary-spread can be triggered by an invasive-procedures (surgery) or by a bone-fracture.In our population we have a case of breast-plasmocytoma diagnosed accidentally after reconstructive breast-surgery,where Polymerase Chain Reaction of immunoglobulin gene-rearrangement in the breast tissue excised confirmed monoclonal-CD 138/lambda plasma-cells. This patients at first was treated with VTD-regimen followed by tandem-ASCT and after EM-relapse achieved complete remission with haploidentical-bone-marrow-transplantation.Allogeneic transplantation should however be remembered in the therapeutic-armamentarium against EM especially in high-risk-young-patients.Furthemore often it has been described in the literature association between EMD, IgD subtype and FLC (free light chain)escape. In fact in our study we have reviewed 6 cases of IgD and 4 FLC-escape, all of them were observed in relapse-setting and in sEMD group.Finally the mechanism of extramedullary spread are poorly established:maybe a decrease expression of integrins and CD56 is involved. In our population absence of CD56 protein was shown in 56% of sEMD group and in 15%of bEMD case-series.
Conclusion
Cinical features of MM-patients with bEMD were different from the patients with sEMD.Outcome of this population was significantly better than the patients with sEMD, and was comparable to the patients without EMD. Even in the era of novel drugs extramedullary soft tissue has a poor prognosis expecially in a relapse-setting.This work shows a significant difference in prognosis for different type of extramedullary-disease even between sEMD(better OS of skin and lymph nodes involvement) suggesting a different biological-behavior.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Outcome, Multiple Myeloma, Extramedullary hematopoiesis
Abstract: PB1953
Type: Publication Only
Background
Extramedullary disease is an uncommon manifestation in multiple myeloma(MM) and can either accompany newly diagnosed disease or develop with disease progression or relapse. Extramedullary myeloma(EMM)seems to have a different pathogenesis from its much more frequently encountered medullary counterpart, showing often a poor prognosis. EMM clinical situations are extraordinarily heterogeneous and their management is challenging.This includes organ or tissue involvement resulting from hematogenous-spread and/or bone involvement originating from different kind of bones.
Aims
We evaluated the impact of this disease features on patients’ outcome in the context of novel-agents.
Methods
We reviewed 84 patients presenting EMM (median age 60, range 30-76)describing clinical and biological features(Table 1).Our aim was studying prognosis of bone-related extramedullary-disease (bEMD) and its relationship with soft-tissue related EMD (sEMD)in MM patients in our institution.
Results
42 bEMD and 42 sEMD patients treated at Our Department between 2007 and 2016 were included in this study. Of the first group 10 presented EMM at diagnosis and 32 at relapse as well as 7 and 35 respectevely of the second series.31 among sEMD were dead and 11 were alive, 20 of bEMD patients were dead and 22 were still alive. EM was diagnosed using imaging techiniques such as PET-CT (35%) or magnetic resonance MRI (65%).Biopsies were carried out only if the lesion was accessible (62%). The treatment was heterogeneous and all patients had receveid either thalidomide or bortezomib in the first-line of therapy. We showed that sEMD cohort has a significantly poorer survival compared to bEMD patients (median OS from diagnosis of EMD of 13 versus 58 months, P<0001). Finally lung, liver (parenchyma-EM)and SNC involvement among sEMD patients has shown a poorer outcome when compared to skin and lymph nodes masses respectively median OS of 12 and 10 months versus 18 and 15 months P <0001). Conversely among bEMD group there wasn’t a significant advantage of outcome regarding the different bones involved. Kaplan-Meier estimates were used for survival analysis and differences between survival-times in patient subgroups were tested using the log-rank test(Figure 1).Interestingly extramedullary-spread can be triggered by an invasive-procedures (surgery) or by a bone-fracture.In our population we have a case of breast-plasmocytoma diagnosed accidentally after reconstructive breast-surgery,where Polymerase Chain Reaction of immunoglobulin gene-rearrangement in the breast tissue excised confirmed monoclonal-CD 138/lambda plasma-cells. This patients at first was treated with VTD-regimen followed by tandem-ASCT and after EM-relapse achieved complete remission with haploidentical-bone-marrow-transplantation.Allogeneic transplantation should however be remembered in the therapeutic-armamentarium against EM especially in high-risk-young-patients.Furthemore often it has been described in the literature association between EMD, IgD subtype and FLC (free light chain)escape. In fact in our study we have reviewed 6 cases of IgD and 4 FLC-escape, all of them were observed in relapse-setting and in sEMD group.Finally the mechanism of extramedullary spread are poorly established:maybe a decrease expression of integrins and CD56 is involved. In our population absence of CD56 protein was shown in 56% of sEMD group and in 15%of bEMD case-series.
Conclusion
Cinical features of MM-patients with bEMD were different from the patients with sEMD.Outcome of this population was significantly better than the patients with sEMD, and was comparable to the patients without EMD. Even in the era of novel drugs extramedullary soft tissue has a poor prognosis expecially in a relapse-setting.This work shows a significant difference in prognosis for different type of extramedullary-disease even between sEMD(better OS of skin and lymph nodes involvement) suggesting a different biological-behavior.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Outcome, Multiple Myeloma, Extramedullary hematopoiesis
{{ help_message }}
{{filter}}


