IMPACT OF RENAL IMPAIRMENT IN NEWLY DIAGNOSED MULTIPLE MYELOMA IN A REAL WORLD SETTING.
(Abstract release date: 05/18/17)
EHA Library. Bove V. 05/18/17; 182663; PB1949

Virginia Bove
Contributions
Contributions
Abstract
Abstract: PB1949
Type: Publication Only
Background
Renal impairment (RI) is a frequent complication of patients with newly diagnosed multiple myeloma (NDMM), reported in 15-40% with 10% requiring hemodialysis (HD). It is associated with higher early mortality (EM) and lower overall survival (OS). Early diagnosis and treatment with new agents improve these results.
Aims
Analyze renal response, OS and EM in NDMM with RI and compare them to patients with MM without RI.
Methods
All consecutive and unselected NDMM patients treated at Hospital de Clínicas, Montevideo, Uruguay, from January 2011 to June 2015 were included. Our database was completed prospectively and included clinical and laboratory characteristics of the disease, treatment, treatment-related adverse events, response, HD requirement, renal response and mortality.
Diagnosis of MM, response to treatment and degree of renal function recovery were based on the International Myeloma Working Group criteria. RI was defined as an estimated glomerular filtration rate (eGFR) <40 ml/min/1.73m2, calculated by MDRD (Modification of Diet in Renal Disease) equation. Patients whose RI was explained by other causes were excluded. Early treatment was defined by initiation within 7 days after diagnosis. EM was defined as death within 3 months of diagnosis.
Results
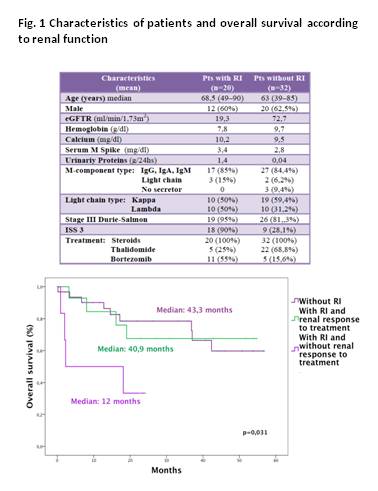
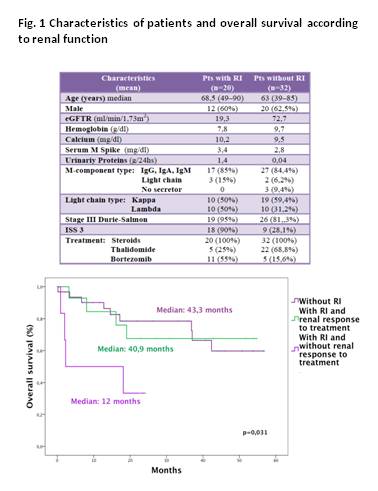
MM was diagnosed in 52 patients, median age was 67 years (range 39-90), 61,5% were male, 38,5% had RI. The characteristics of the patients and front-line treatment are shown in Fig 1. Overall response to first line treatment was 70% for those with RI (CR 20%) and 68,8% in patients without RI (CR 15,4%). Treatment related adverse effects were higher in patients with RI (45% vs 28,2%), being polyneuropathy the most common side effect. Patients with RI required more dose adjustments (40% vs 6,3%).
Renal response: 50% reversed RI, 10% achieved renal PR and 40% renal CR, all before the 4th month from diagnosis; 77,8% started early treatment and 70% received bortezomib (bz). Patients whose RI did not reverse had had late initiation of treatment in 78% and 40% received bz. Six patients (30%) remained in chronic HD, all had late initiation of treatment. Two of the 6 patients who required HD at diagnosis obtained later independence; both received bz and one was consolidated with autologous stem cell transplantation.
Impact of RI on OS and EM: median OS in patients with RI was not significatively different to that of MM without RI (35,3 vs 43,3 months, p=0,346). Patients without RI had higher OS compared to those who had reversible renal failure and those who never recovered (43,3; 40,9 and 12 months, respectively, p=0,031). OS was higher in patients with RI who received bz vs other therapeutic schemes (42,5 vs 25,8 months, p=0,137). With a mean follow-up of 26 months, mortality was 40% and 28,1% in patients with and without RI, respectively. EM were also higher in patients with RI at diagnosis (50% vs 22,5%). The main cause of EM was infection in both groups.
Conclusion
RI was frequent in NDMM and was associated with advanced disease and higher tumor mass (>90% stage III Durie-Salmon and ISS3), revealing a late diagnosis. Prompt institution of treatment and use of bz relates to higher recovery of renal function and dyalisis independence. Although toxicity and dose adjustements were higher in patients with RI this was not associated with lower response to treatment. Reversal of renal failure associates with better OS, similar to those without RI at diagnosis. EM are more prevalent in patients with RI at diagnosis.
Even when the number of patients is small, this real life data supports the need of planning local strategies that lead to early diagnosis and initiation of treatment, which are crucial to reduce morbidity and mortality associated to RI in NDMM.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Renal impairment, Multiple Myeloma
Abstract: PB1949
Type: Publication Only
Background
Renal impairment (RI) is a frequent complication of patients with newly diagnosed multiple myeloma (NDMM), reported in 15-40% with 10% requiring hemodialysis (HD). It is associated with higher early mortality (EM) and lower overall survival (OS). Early diagnosis and treatment with new agents improve these results.
Aims
Analyze renal response, OS and EM in NDMM with RI and compare them to patients with MM without RI.
Methods
All consecutive and unselected NDMM patients treated at Hospital de Clínicas, Montevideo, Uruguay, from January 2011 to June 2015 were included. Our database was completed prospectively and included clinical and laboratory characteristics of the disease, treatment, treatment-related adverse events, response, HD requirement, renal response and mortality.
Diagnosis of MM, response to treatment and degree of renal function recovery were based on the International Myeloma Working Group criteria. RI was defined as an estimated glomerular filtration rate (eGFR) <40 ml/min/1.73m2, calculated by MDRD (Modification of Diet in Renal Disease) equation. Patients whose RI was explained by other causes were excluded. Early treatment was defined by initiation within 7 days after diagnosis. EM was defined as death within 3 months of diagnosis.
Results
MM was diagnosed in 52 patients, median age was 67 years (range 39-90), 61,5% were male, 38,5% had RI. The characteristics of the patients and front-line treatment are shown in Fig 1. Overall response to first line treatment was 70% for those with RI (CR 20%) and 68,8% in patients without RI (CR 15,4%). Treatment related adverse effects were higher in patients with RI (45% vs 28,2%), being polyneuropathy the most common side effect. Patients with RI required more dose adjustments (40% vs 6,3%).
Renal response: 50% reversed RI, 10% achieved renal PR and 40% renal CR, all before the 4th month from diagnosis; 77,8% started early treatment and 70% received bortezomib (bz). Patients whose RI did not reverse had had late initiation of treatment in 78% and 40% received bz. Six patients (30%) remained in chronic HD, all had late initiation of treatment. Two of the 6 patients who required HD at diagnosis obtained later independence; both received bz and one was consolidated with autologous stem cell transplantation.
Impact of RI on OS and EM: median OS in patients with RI was not significatively different to that of MM without RI (35,3 vs 43,3 months, p=0,346). Patients without RI had higher OS compared to those who had reversible renal failure and those who never recovered (43,3; 40,9 and 12 months, respectively, p=0,031). OS was higher in patients with RI who received bz vs other therapeutic schemes (42,5 vs 25,8 months, p=0,137). With a mean follow-up of 26 months, mortality was 40% and 28,1% in patients with and without RI, respectively. EM were also higher in patients with RI at diagnosis (50% vs 22,5%). The main cause of EM was infection in both groups.
Conclusion
RI was frequent in NDMM and was associated with advanced disease and higher tumor mass (>90% stage III Durie-Salmon and ISS3), revealing a late diagnosis. Prompt institution of treatment and use of bz relates to higher recovery of renal function and dyalisis independence. Although toxicity and dose adjustements were higher in patients with RI this was not associated with lower response to treatment. Reversal of renal failure associates with better OS, similar to those without RI at diagnosis. EM are more prevalent in patients with RI at diagnosis.
Even when the number of patients is small, this real life data supports the need of planning local strategies that lead to early diagnosis and initiation of treatment, which are crucial to reduce morbidity and mortality associated to RI in NDMM.
Session topic: 14. Myeloma and other monoclonal gammopathies - Clinical
Keyword(s): Renal impairment, Multiple Myeloma
{{ help_message }}
{{filter}}


