
Contributions
Abstract: PB1905
Type: Publication Only
Background
Aims
The aim of the present study was to evaluate the frequency and extent of hyperferritinemia as well as serum concentrations of selected inflammatory cytokines at the time of diagnosis of hematological malignancy-associated HLH (hM-HLH) in adults.
Methods
Results
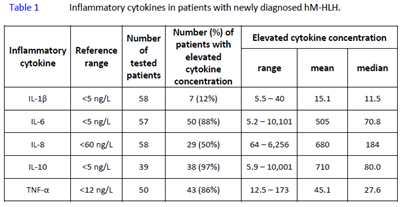
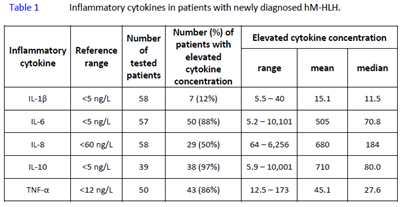
Lymphoid malignancy was diagnosed in 42 patients and myeloid malignancy in 29 patients. Fifty-four (76%) patients developed HLH as a first manifestation of an unknown malignancy, during progressive disease, or at malignancy relapse. The remaining 24% of patients developed HLH during chemotherapy. Serum ferritin concentration (ref.: 30–350 μg/L) at the time of hM-HLH diagnosis was elevated in all but one patient (70/71, 98%). Mean ferritinemia was 37,281±84,440 μg/L, median value 14,727 μg/L, and ferritinemia range 96–645,291 µg/L. As HLH-2004 criterion, hyperferritinemia ≥500 µg/L was present in 69 of 71 patients (97%) at the time of HLH diagnosis. Hyperferritinemia of ≥2000 µg/L was noted in 67 (94%) patients, hyperferritinemia of ≥5000 µg/L in 56 (79%) patients, and hyperferritinemia of ≥10,000 µg/L occured in 42 (59%) patients. Serum levels of sIL-2Rα (sCD25) were measured in 69/71 patients, of whom 91% (63/69) had values ≥2400 U/mL. Moreover, in 3 more patients sIL-2Rα was clearly elevated to 2179, 2233, and 2345 U/mL, respectively. Concentrations of TNF-α, IL-6, and IL-10 in serum were each elevated in over 85% of the examined hM-HLH patients. IL-8 concentration was increased in half of all tested patients at the time of HLH diagnosis. However, IL-1β concentration was above reference range only in 12% of patients (7 of 58). Results of the inflammatory cytokine analyses in patients with newly diagnosed hM-HLH are presented in Table.
Conclusion
Session topic: 28. Iron metabolism, deficiency and overload
Keyword(s): Malignancy, Ferritin, Cytokine
Abstract: PB1905
Type: Publication Only
Background
Aims
The aim of the present study was to evaluate the frequency and extent of hyperferritinemia as well as serum concentrations of selected inflammatory cytokines at the time of diagnosis of hematological malignancy-associated HLH (hM-HLH) in adults.
Methods
Results
Lymphoid malignancy was diagnosed in 42 patients and myeloid malignancy in 29 patients. Fifty-four (76%) patients developed HLH as a first manifestation of an unknown malignancy, during progressive disease, or at malignancy relapse. The remaining 24% of patients developed HLH during chemotherapy. Serum ferritin concentration (ref.: 30–350 μg/L) at the time of hM-HLH diagnosis was elevated in all but one patient (70/71, 98%). Mean ferritinemia was 37,281±84,440 μg/L, median value 14,727 μg/L, and ferritinemia range 96–645,291 µg/L. As HLH-2004 criterion, hyperferritinemia ≥500 µg/L was present in 69 of 71 patients (97%) at the time of HLH diagnosis. Hyperferritinemia of ≥2000 µg/L was noted in 67 (94%) patients, hyperferritinemia of ≥5000 µg/L in 56 (79%) patients, and hyperferritinemia of ≥10,000 µg/L occured in 42 (59%) patients. Serum levels of sIL-2Rα (sCD25) were measured in 69/71 patients, of whom 91% (63/69) had values ≥2400 U/mL. Moreover, in 3 more patients sIL-2Rα was clearly elevated to 2179, 2233, and 2345 U/mL, respectively. Concentrations of TNF-α, IL-6, and IL-10 in serum were each elevated in over 85% of the examined hM-HLH patients. IL-8 concentration was increased in half of all tested patients at the time of HLH diagnosis. However, IL-1β concentration was above reference range only in 12% of patients (7 of 58). Results of the inflammatory cytokine analyses in patients with newly diagnosed hM-HLH are presented in Table.
Conclusion
Session topic: 28. Iron metabolism, deficiency and overload
Keyword(s): Malignancy, Ferritin, Cytokine


