
Contributions
Abstract: PB1883
Type: Publication Only
Background
Ocular adnexal lymphoma (OAL) accounts for 1-2% of Non-Hodgkin Lymphomas (NHL) and 8% of all extra-nodal sites. The majority of cases, >95%, are of B cell origin and 80% are low grade lymphomas. Secondary ocular involvement occurs in approximately 2.4-5.3% of patients with advanced systemic NHL. Marginal zone lymphoma or mucosa-associated lymphoid tissue (MALT) lymphoma is reported in approximately 50% of patients. Current treatment options for low grade OAL include radiotherapy and chemotherapy. Chlamydia Psittaci DNA has been reported in up to 80% of tumor biopsies from patients with OAL suggesting a possible value of anti-Chlamydia Psittaci antibiotic therapy.
Aims
To report a single centre’s experience in the outcomes of patients diagnosed with OAL over a 13 year period.
Methods
A Retrospective cohort of patients with low grade OAL treated in a single Centre between 2003 and 2016 was analyzed. Chemotherapy was the first choice of therapy until 2008, afterwards radiotherapy became the first line treatment for OAL.
Results
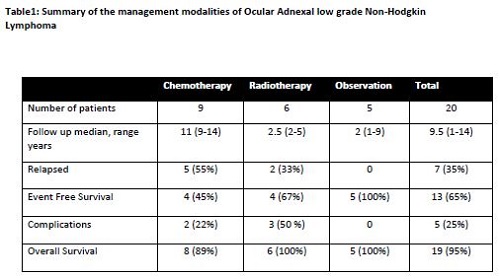
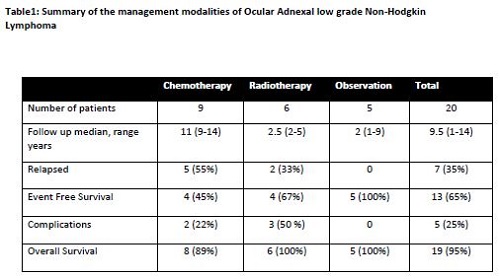
A total of 20 patients with OAL were identified. 60% (12/20) of patients were females with a median age of 61.5 years (range 45-85 years). 80 %( 16/20) had unilateral disease at presentation. MALT lymphomas comprised 75 %( 15/20), Follicular NHL 15% and CLL/SLL 10%. Only 10% (2/20) had a prior diagnosis of NHL. At presentation 20% (4/20) had evidence of systemic involvement: 19% (3/16) had bone marrow involvement and 1 patient had small volume lymphadenopathy on CT scan. 45% (9/20) were treated with first line chemotherapy, single agent Chlorambucil in 78% (7/9) and 2 patients received Fludarabine based chemotherapy, 30% (6/20) received first line radiotherapy, 24Gy in 12 fractions in 67% (4/6), and 25% (6/20) were managed under observation. In the chemotherapy group 55% (5/9) experienced 1 relapse (3/5 local recurrence and 2/5 extra-ocular relapse), 3 patients experienced ≥2 relapses, 2 patients had disease transformation to high grade and 1 patient subsequently died as a consequence of their disease. 33% (2/6) patients treated with radiotherapy experienced disease recurrence, mainly extra-ocular and 50% (3/6) suffered complications following radiotherapy in the form of dry eyes and cataract. Median follow up was 9.5 years (range 1-14 years). Overall survival was 95% (19/20) with an event free survival of 65% (13/20).
Conclusion
The majority of patients in our cohort had favorable outcomes. Currently there is no national guideline for the management of OAL in the UK. Several treatment options exist including chemotherapy, radiotherapy, immunotherapy, observation or more recently the use of eradication treatment for Chlamydia Psittaci. Factors to consider when choosing a treatment include a patient’s co-morbidities, risk of visual impairment, need for systemic therapy, histological diagnosis and anticipated side effects. As treatments are so effective the long term consequences and possible late effects need to be acknowledged and avoided if at all possible. Observation is an acceptable approach in asymptomatic patients when there is no immediate risk of visual impairment. Radiotherapy is an effective first line treatment in symptomatic and localized OAL, the exact dose of radiotherapy to achieve disease control with minimal long term side effects is yet to be determined. Reviews with larger number of patients are needed to inform a practical approach to the management of OAL.
Session topic: 19. Indolent Non-Hodgkin lymphoma - Clinical
Keyword(s): Radiotherapy, Low-grade NHL, chemotherapy
Abstract: PB1883
Type: Publication Only
Background
Ocular adnexal lymphoma (OAL) accounts for 1-2% of Non-Hodgkin Lymphomas (NHL) and 8% of all extra-nodal sites. The majority of cases, >95%, are of B cell origin and 80% are low grade lymphomas. Secondary ocular involvement occurs in approximately 2.4-5.3% of patients with advanced systemic NHL. Marginal zone lymphoma or mucosa-associated lymphoid tissue (MALT) lymphoma is reported in approximately 50% of patients. Current treatment options for low grade OAL include radiotherapy and chemotherapy. Chlamydia Psittaci DNA has been reported in up to 80% of tumor biopsies from patients with OAL suggesting a possible value of anti-Chlamydia Psittaci antibiotic therapy.
Aims
To report a single centre’s experience in the outcomes of patients diagnosed with OAL over a 13 year period.
Methods
A Retrospective cohort of patients with low grade OAL treated in a single Centre between 2003 and 2016 was analyzed. Chemotherapy was the first choice of therapy until 2008, afterwards radiotherapy became the first line treatment for OAL.
Results
A total of 20 patients with OAL were identified. 60% (12/20) of patients were females with a median age of 61.5 years (range 45-85 years). 80 %( 16/20) had unilateral disease at presentation. MALT lymphomas comprised 75 %( 15/20), Follicular NHL 15% and CLL/SLL 10%. Only 10% (2/20) had a prior diagnosis of NHL. At presentation 20% (4/20) had evidence of systemic involvement: 19% (3/16) had bone marrow involvement and 1 patient had small volume lymphadenopathy on CT scan. 45% (9/20) were treated with first line chemotherapy, single agent Chlorambucil in 78% (7/9) and 2 patients received Fludarabine based chemotherapy, 30% (6/20) received first line radiotherapy, 24Gy in 12 fractions in 67% (4/6), and 25% (6/20) were managed under observation. In the chemotherapy group 55% (5/9) experienced 1 relapse (3/5 local recurrence and 2/5 extra-ocular relapse), 3 patients experienced ≥2 relapses, 2 patients had disease transformation to high grade and 1 patient subsequently died as a consequence of their disease. 33% (2/6) patients treated with radiotherapy experienced disease recurrence, mainly extra-ocular and 50% (3/6) suffered complications following radiotherapy in the form of dry eyes and cataract. Median follow up was 9.5 years (range 1-14 years). Overall survival was 95% (19/20) with an event free survival of 65% (13/20).
Conclusion
The majority of patients in our cohort had favorable outcomes. Currently there is no national guideline for the management of OAL in the UK. Several treatment options exist including chemotherapy, radiotherapy, immunotherapy, observation or more recently the use of eradication treatment for Chlamydia Psittaci. Factors to consider when choosing a treatment include a patient’s co-morbidities, risk of visual impairment, need for systemic therapy, histological diagnosis and anticipated side effects. As treatments are so effective the long term consequences and possible late effects need to be acknowledged and avoided if at all possible. Observation is an acceptable approach in asymptomatic patients when there is no immediate risk of visual impairment. Radiotherapy is an effective first line treatment in symptomatic and localized OAL, the exact dose of radiotherapy to achieve disease control with minimal long term side effects is yet to be determined. Reviews with larger number of patients are needed to inform a practical approach to the management of OAL.
Session topic: 19. Indolent Non-Hodgkin lymphoma - Clinical
Keyword(s): Radiotherapy, Low-grade NHL, chemotherapy


