
Contributions
Abstract: PB1787
Type: Publication Only
Background
The inclusion in the treatment program of new drugs (including new monoclonal antibodies and targeted therapies) allowed the majority of patients with chronic lymphocytic leukemia (CLL) to achieve disease remission (complete or partial) after combined therapy. So, at now, the urgent task is long-term preservation and the deepening of the therapeutic response, if it is possible. This problem can be solved by intensification of therapy (including autologous transplantation of hematopoietic stem cells) or maintenance therapy (MT)
Aims
To estimate the importance of maintenance therapy in the treatment of patients with CLL
Methods
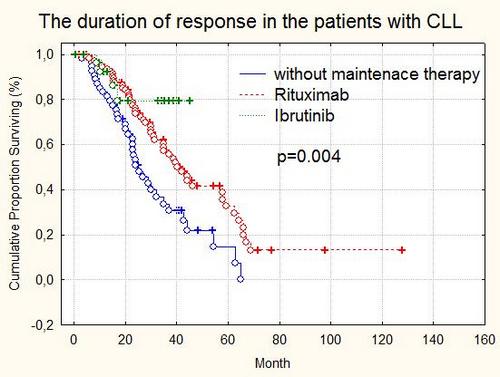
The study included 198 patients. Male to female ratio - 1.3:1. We have used NCI revised guidelines (Hallek M, et al., 2008) for treatment initiation, assessment of response and minimal residual disease (MRD). Induction chemotherapy was conducted under the following programs: RB, FC, RFC, R-CHOP, Ibrutinib-RB, Ibrutinib-R. Evaluation of MRD was performed using 5-color flow cytometry of the bone marrow cells. The maintenance therapy was conducted 144 (72.7%) patients: Rituximab 500 mg/m2 intravenously every 8 weeks (n=116) for 2 years; Ibrutinib 420 mg, orally, daily (n=28) continuously. The remaining patients (n=54) were under dynamic observation without therapy
Results
Conclusion
The conducting of MT patients with CLL allows to achieve increasing the depth achieved remission and increase the duration of its preservation. MT may be a means of control over the minimal residual disease and the method of its eradication
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): Maintenance, Chronic Lymphocytic Leukemia, Targeted therapy, Minimal residual disease (MRD)
Abstract: PB1787
Type: Publication Only
Background
The inclusion in the treatment program of new drugs (including new monoclonal antibodies and targeted therapies) allowed the majority of patients with chronic lymphocytic leukemia (CLL) to achieve disease remission (complete or partial) after combined therapy. So, at now, the urgent task is long-term preservation and the deepening of the therapeutic response, if it is possible. This problem can be solved by intensification of therapy (including autologous transplantation of hematopoietic stem cells) or maintenance therapy (MT)
Aims
To estimate the importance of maintenance therapy in the treatment of patients with CLL
Methods
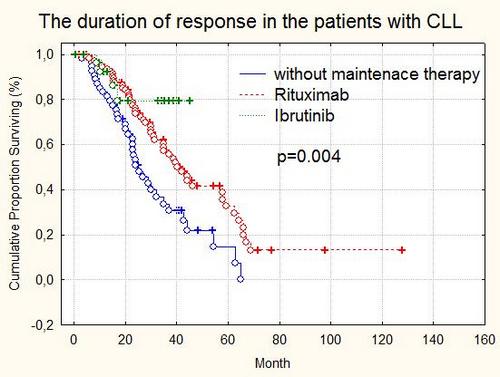
The study included 198 patients. Male to female ratio - 1.3:1. We have used NCI revised guidelines (Hallek M, et al., 2008) for treatment initiation, assessment of response and minimal residual disease (MRD). Induction chemotherapy was conducted under the following programs: RB, FC, RFC, R-CHOP, Ibrutinib-RB, Ibrutinib-R. Evaluation of MRD was performed using 5-color flow cytometry of the bone marrow cells. The maintenance therapy was conducted 144 (72.7%) patients: Rituximab 500 mg/m2 intravenously every 8 weeks (n=116) for 2 years; Ibrutinib 420 mg, orally, daily (n=28) continuously. The remaining patients (n=54) were under dynamic observation without therapy
Results
Conclusion
The conducting of MT patients with CLL allows to achieve increasing the depth achieved remission and increase the duration of its preservation. MT may be a means of control over the minimal residual disease and the method of its eradication
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): Maintenance, Chronic Lymphocytic Leukemia, Targeted therapy, Minimal residual disease (MRD)


