FETAL INTRACRANIAL HEMORRHAGE AS A PRESENTING FEATURE OF SEVERE CONGENITAL FACTOR VII DEFICIENCY: THE NEED FOR EARLY PROPHYLAXIS
(Abstract release date: 05/18/17)
EHA Library. Elshinawy M. 05/18/17; 182463; PB1749

Assoc. Prof. Mohamed Elshinawy
Contributions
Contributions
Abstract
Abstract: PB1749
Type: Publication Only
Background
Congenital factor VII (FVII) deficiency is a rare autosomal recessive bleeding disorder, with an estimated prevalence of 1:300,000. Compared to western countries, rare bleeding disorders (RBDs) are relatively commoner in Oman, owing to high rate of consanguineous marriage.
Aims
To discuss an interesting case fo severe congenital factor VII deficiency and to explore the need for early prophylaxis.
Methods
Case report and retrospective data analysis of all children diagnosed with inherited coagulation factor deficiencies in Pediatric Hematology Unit, Sultan Qaboos University Hospital, Muscat, Oman from January 2009 till December 2016.
Results
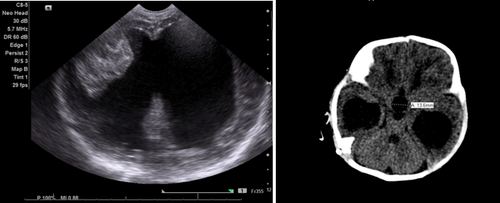
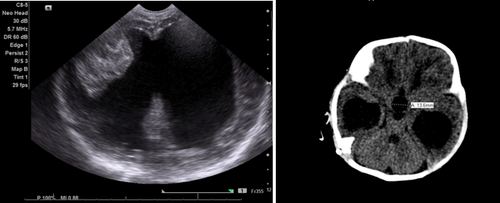
We report a male full term baby, delivered by cesarean section. His older sister is a known case of severe congenital factor VII deficiency. Antenatal scans of this baby revealed two intracerebral hematomas and dilated cerebral ventricles. Postnatally, the diagnosis of severe congenital FVII deficiency was confirmed. CT scan revealed obstructive hydrocephalus at the level of aqueduct of Sylvius (figure 1). At day 10 of life, ventriculo-peritoneal shunt has been done successfully under cover of recombinant activated factor VII replacement therapy. Afterwards, the patient has been initiated on rFVIIa prophylaxis at a dose of 30 ug/kg three times weekly. In our center, deficiencies of fibrinogen, FV, FVII, FX and FXIII were diagnosed in 22 pediatric patients (10 males and 12 females), accounting for 11.1 % (22/198) of all children with inherited coagulation factor deficiencies. The age ranges from 1 day to 6 years and consanguinity is found in 19/22 cases (86.4%). Hypofibrinogenemia, FV and FVII deficiency are the commonest RBDs, diagnosed in 8, 6 and 5 patients respectively. As an initial presentation, intracranial hemorrhage occurred in 7/22 cases (31.8%). Three patients with FV, FVII and FXIII deficiencies suffered from global developmental delay due to severe intracranial hemorrhage. As regards management, 4 patients with severe FV deficiency and one with severe FXIII deficiency are on fresh frozen plasma (FFP) and recombinant FXIII prophylaxis respectively. Other patients receive on-demand therapy.
Conclusion
Children with RBDs constitute more than one tenth of cases of hereditary coagulation factor deficiencies in our center. They have some unique features in terms of severity, clinical profile and the need for prophylaxis early in life. We recommend establishing a national/regional registry of RBDs to identify the magnitude and the peculiar genotype-phenotype correlations of such rare, yet significant disorders.
Session topic: 33. Bleeding disorders (congenital and acquired)
Keyword(s): Factor VIIa, Coagulation factors
Abstract: PB1749
Type: Publication Only
Background
Congenital factor VII (FVII) deficiency is a rare autosomal recessive bleeding disorder, with an estimated prevalence of 1:300,000. Compared to western countries, rare bleeding disorders (RBDs) are relatively commoner in Oman, owing to high rate of consanguineous marriage.
Aims
To discuss an interesting case fo severe congenital factor VII deficiency and to explore the need for early prophylaxis.
Methods
Case report and retrospective data analysis of all children diagnosed with inherited coagulation factor deficiencies in Pediatric Hematology Unit, Sultan Qaboos University Hospital, Muscat, Oman from January 2009 till December 2016.
Results
We report a male full term baby, delivered by cesarean section. His older sister is a known case of severe congenital factor VII deficiency. Antenatal scans of this baby revealed two intracerebral hematomas and dilated cerebral ventricles. Postnatally, the diagnosis of severe congenital FVII deficiency was confirmed. CT scan revealed obstructive hydrocephalus at the level of aqueduct of Sylvius (figure 1). At day 10 of life, ventriculo-peritoneal shunt has been done successfully under cover of recombinant activated factor VII replacement therapy. Afterwards, the patient has been initiated on rFVIIa prophylaxis at a dose of 30 ug/kg three times weekly. In our center, deficiencies of fibrinogen, FV, FVII, FX and FXIII were diagnosed in 22 pediatric patients (10 males and 12 females), accounting for 11.1 % (22/198) of all children with inherited coagulation factor deficiencies. The age ranges from 1 day to 6 years and consanguinity is found in 19/22 cases (86.4%). Hypofibrinogenemia, FV and FVII deficiency are the commonest RBDs, diagnosed in 8, 6 and 5 patients respectively. As an initial presentation, intracranial hemorrhage occurred in 7/22 cases (31.8%). Three patients with FV, FVII and FXIII deficiencies suffered from global developmental delay due to severe intracranial hemorrhage. As regards management, 4 patients with severe FV deficiency and one with severe FXIII deficiency are on fresh frozen plasma (FFP) and recombinant FXIII prophylaxis respectively. Other patients receive on-demand therapy.
Conclusion
Children with RBDs constitute more than one tenth of cases of hereditary coagulation factor deficiencies in our center. They have some unique features in terms of severity, clinical profile and the need for prophylaxis early in life. We recommend establishing a national/regional registry of RBDs to identify the magnitude and the peculiar genotype-phenotype correlations of such rare, yet significant disorders.
Session topic: 33. Bleeding disorders (congenital and acquired)
Keyword(s): Factor VIIa, Coagulation factors
{{ help_message }}
{{filter}}


