
Contributions
Abstract: PB1705
Type: Publication Only
Background
DLBCL is the most common histologic subtype of non-Hodgkin lymphoma (NHL), accounting for about 33% of all NHL cases. However, the healthcare burden associated with DLBCL has not been extensively studied in a US population.
Aims
We evaluated the costs of care and healthcare utilization (HCU) of DLBCL patients treated during routine care in the US.
Methods
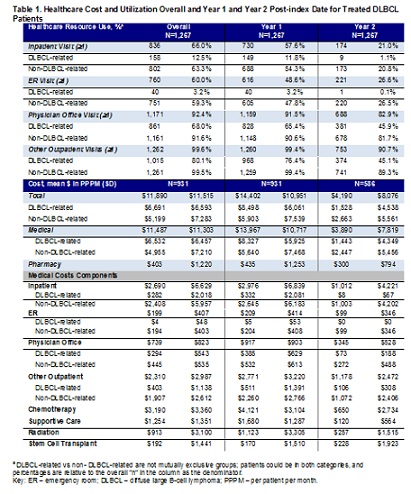
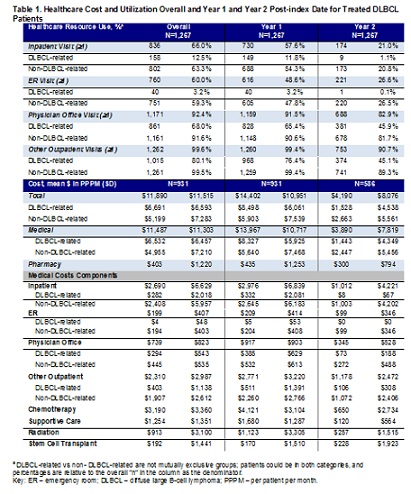
Results
Conclusion
The economic burden associated with the treated DLBCL population is high, with the majority of costs incurred during the first year of diagnosis. Between the first and second year of diagnosis, costs decrease mainly because of the decrease in the DLBCL-related treatment costs. In addition, HCU for DLBCL-related services decreased in Year 1 vs Year 2.
Session topic: 20. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Health care, Diffuse large B cell lymphoma, Cost analysis
Abstract: PB1705
Type: Publication Only
Background
DLBCL is the most common histologic subtype of non-Hodgkin lymphoma (NHL), accounting for about 33% of all NHL cases. However, the healthcare burden associated with DLBCL has not been extensively studied in a US population.
Aims
We evaluated the costs of care and healthcare utilization (HCU) of DLBCL patients treated during routine care in the US.
Methods
Results
Conclusion
The economic burden associated with the treated DLBCL population is high, with the majority of costs incurred during the first year of diagnosis. Between the first and second year of diagnosis, costs decrease mainly because of the decrease in the DLBCL-related treatment costs. In addition, HCU for DLBCL-related services decreased in Year 1 vs Year 2.
Session topic: 20. Aggressive Non-Hodgkin lymphoma - Clinical
Keyword(s): Health care, Diffuse large B cell lymphoma, Cost analysis


