IS HIF-2 ALPHA A POOR PROGNOSIS FACTOR IN HUMAN ACUTE MYELOID LEUKEMIA? A SINGLE CENTER ANALYSIS - PRELIMINARY RESULTS
(Abstract release date: 05/18/17)
EHA Library. Dybko J. 05/18/17; 182409; PB1695

Jaroslaw Dybko
Contributions
Contributions
Abstract
Abstract: PB1695
Type: Publication Only
Background
Hypoxia-inducible transcription factors (HIF) are well known regulators of cellular response to hypoxia. HIFs control functional, metabolic and vascular adaptation to hypoxia on transcriptional level. HIF-1 alpha has been also described to be responsible for solid tumors chemoresistance, invasion, metastasis and relapse. The role of HIFs in leukemias has not been established well so far. First reports of poor outcomes of antileukemic treatment linked with overexpression of HIF-1α has been published. Moreover another HIF subunit - HIF-2 alpha - has been described in mouse model as increasing myeloid preleukemic cell proliferation and accelerating disease progression with reduced survival. On this background, we found interesting if HIF-s alpha expression in acute myeloid leukemia cells (AML) influences the prognosis in human. We have tried to find a connection between AML cells percentage expressing HIF-2 alpha and first line chemotherapy results.
Aims
The aim of the study was to determine the roole of HIF-2 alpha in human AML
Methods
We analyzed a 26 primary AML patients group (median age 54.5 (21-77), F/M – 13/13). The group consisted of 21 AML-NOS cases, 2 AML cases with inv(16), one case with t(6;9) and one with t(9;11) according WHO classification. ELN cytogenetic risk stratification divided the group into intermdiate-1, intermediate-2 and adverse cases in 10, 12 and 4 patients respectively. All patients were treated with Daunorubicine, Cytarabine and Cladribine based first line chemotherapy. We collect bone marrow and blood samples before chemotherapy and blood samples alone 48 hours after chemotherapy start. In all samples leukemic blasts were counted and determined by flow cytometry and the subpopulation of HIF-2 alpha positive blasts was estimated as well. Volunteer bone marrow donors were the control group in this study and the CD34+HIF-2α+ subpopulation was assessed in their bone marrow samples during the routine harvest procedure. The study was approved by the local Ethics Committee.
Results
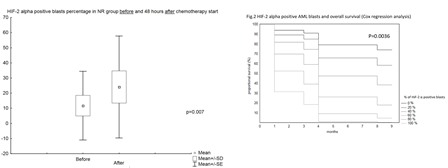
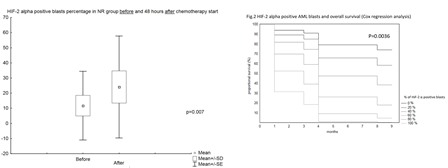
After the first line chemotherapy 15 patients achieved complete remission (CR group) and 11 did not (NR group). We did not find significant differences between the groups regarding patients age, the mean percentage of blasts in bone marrow and blood before the treatment, the percentage of HIF-2 alpha positive blasts in BM and blood before and 48 hours after the treatment start (data not shown). But the analysis of the percentage of HIF-2 alpha positive blasts in blood before and 48 hours separately in CR and NR groups revealed quite different dynamics. In CR group the mean percentage of HIF-2 alpha positive blasts was 14.65 (±33.32) and 8.48 (±11.63) before and after chemotherapy respectively (p=NS); in NR group the values were 11.74 (±22.6) and 24.01 (±33.68) respectively (p=0.007) [Fig.1]. The Cox analysis revealed HIF-2 alpha positive blasts in blood after chemotherapy to be proportional to death probability (p=0.0036) [Fig.2].
Conclusion
We are aware our results are preliminary. But if they are confirmed it will be very interesting to determine the role of HIF-2 alpha inhibitors in improving the prognosis and survival in human AML.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia
Abstract: PB1695
Type: Publication Only
Background
Hypoxia-inducible transcription factors (HIF) are well known regulators of cellular response to hypoxia. HIFs control functional, metabolic and vascular adaptation to hypoxia on transcriptional level. HIF-1 alpha has been also described to be responsible for solid tumors chemoresistance, invasion, metastasis and relapse. The role of HIFs in leukemias has not been established well so far. First reports of poor outcomes of antileukemic treatment linked with overexpression of HIF-1α has been published. Moreover another HIF subunit - HIF-2 alpha - has been described in mouse model as increasing myeloid preleukemic cell proliferation and accelerating disease progression with reduced survival. On this background, we found interesting if HIF-s alpha expression in acute myeloid leukemia cells (AML) influences the prognosis in human. We have tried to find a connection between AML cells percentage expressing HIF-2 alpha and first line chemotherapy results.
Aims
The aim of the study was to determine the roole of HIF-2 alpha in human AML
Methods
We analyzed a 26 primary AML patients group (median age 54.5 (21-77), F/M – 13/13). The group consisted of 21 AML-NOS cases, 2 AML cases with inv(16), one case with t(6;9) and one with t(9;11) according WHO classification. ELN cytogenetic risk stratification divided the group into intermdiate-1, intermediate-2 and adverse cases in 10, 12 and 4 patients respectively. All patients were treated with Daunorubicine, Cytarabine and Cladribine based first line chemotherapy. We collect bone marrow and blood samples before chemotherapy and blood samples alone 48 hours after chemotherapy start. In all samples leukemic blasts were counted and determined by flow cytometry and the subpopulation of HIF-2 alpha positive blasts was estimated as well. Volunteer bone marrow donors were the control group in this study and the CD34+HIF-2α+ subpopulation was assessed in their bone marrow samples during the routine harvest procedure. The study was approved by the local Ethics Committee.
Results
After the first line chemotherapy 15 patients achieved complete remission (CR group) and 11 did not (NR group). We did not find significant differences between the groups regarding patients age, the mean percentage of blasts in bone marrow and blood before the treatment, the percentage of HIF-2 alpha positive blasts in BM and blood before and 48 hours after the treatment start (data not shown). But the analysis of the percentage of HIF-2 alpha positive blasts in blood before and 48 hours separately in CR and NR groups revealed quite different dynamics. In CR group the mean percentage of HIF-2 alpha positive blasts was 14.65 (±33.32) and 8.48 (±11.63) before and after chemotherapy respectively (p=NS); in NR group the values were 11.74 (±22.6) and 24.01 (±33.68) respectively (p=0.007) [Fig.1]. The Cox analysis revealed HIF-2 alpha positive blasts in blood after chemotherapy to be proportional to death probability (p=0.0036) [Fig.2].
Conclusion
We are aware our results are preliminary. But if they are confirmed it will be very interesting to determine the role of HIF-2 alpha inhibitors in improving the prognosis and survival in human AML.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Acute Myeloid Leukemia
{{ help_message }}
{{filter}}


