
Contributions
Abstract: PB1692
Type: Publication Only
Background
A variety of different treatment regimens have been studied in an effort to improve outcomes of patients with relapsed or refractory acute myeloid leukemia (RR-AML), there appears to be no single superior approach. Spanish groups usually use the FLAG-IDA protocol (Fludarabine 30 mg/m2 days 1-4, Idarubicine 12 mg/m2 days 1-3, ara-C 2 mg/m2 days 1-5) in these patients.
Aims
To evaluate our response rates and the survival with FLAG-IDA protocol.
Methods
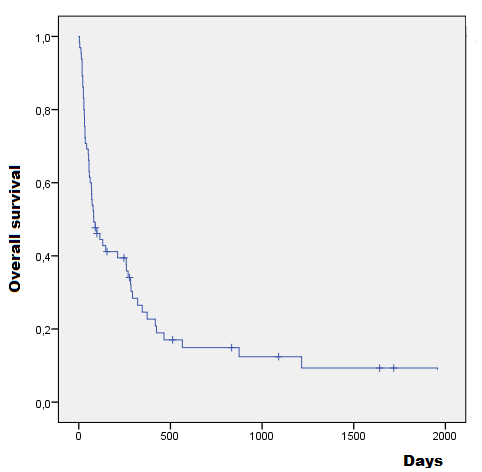
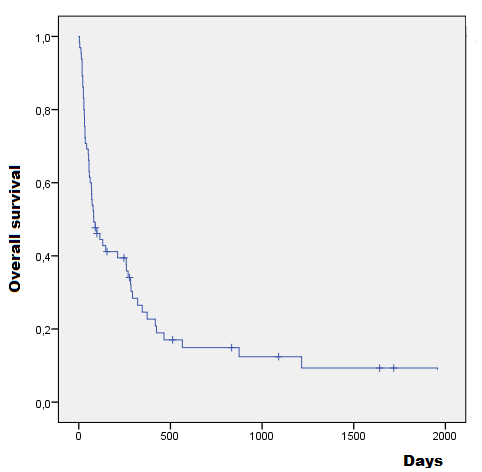
Descriptive study of a case series of patients with acute leukemia who received intensive induction chemotherapy with FLAG-IDA protocol at our hospital between January 2007 and December 2016. Biodemographic, histopathological, cytogenetic and molecular results and previous treatment were recorded. We analyzed the response rate, the 30-day mortality rate and the overall survival.
Results
65 patients received treatment with FLAG-IDA protocol between 2007-2016, 36 of them female, with and average age of 53.4 years (DS+/-23.3). We treated with this protocol mostly patients with relapsed or refractory acute myeloid leukemia (RR-AML) (primary refractory or resistant AML as defined by not achieving complete remission after 1 cycle of intense induction therapy); 60% (n=38) of patients had a RR-AML, 37% (n=23) of them were relapsed AML and 23% (n=15) refractory AML. Based on European Prognostic Index Score (EPI-SCORE) for patients with RR-AML, 61% of them had a poor prognosis (10-14 points), 36% had an intermediate prognosis (7-9 points) and only 3% had a favorable prognosis (1-6 points). The next important group, 25% (n=17) were MDS patients transformed to AML. We had 9% (n=6) patients with treatment related AML and 6% with other acute leukemia (3 cases of refractory ALL and 1 case of biphenotypic leukemia).
Conclusion
Most AML patients ultimately die from their disease. In our case serie none died by any other cause. We had a similar response rate, mortality and overall survival that other groups in our country. Despite a variety of salvage therapy options, like FLAG-IDA protocol, prognosis in patients with RR-AML is generally poor and treatment is very complex.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): acute leukemia, Fludarabine, Ara-C (cytarabine)
Abstract: PB1692
Type: Publication Only
Background
A variety of different treatment regimens have been studied in an effort to improve outcomes of patients with relapsed or refractory acute myeloid leukemia (RR-AML), there appears to be no single superior approach. Spanish groups usually use the FLAG-IDA protocol (Fludarabine 30 mg/m2 days 1-4, Idarubicine 12 mg/m2 days 1-3, ara-C 2 mg/m2 days 1-5) in these patients.
Aims
To evaluate our response rates and the survival with FLAG-IDA protocol.
Methods
Descriptive study of a case series of patients with acute leukemia who received intensive induction chemotherapy with FLAG-IDA protocol at our hospital between January 2007 and December 2016. Biodemographic, histopathological, cytogenetic and molecular results and previous treatment were recorded. We analyzed the response rate, the 30-day mortality rate and the overall survival.
Results
65 patients received treatment with FLAG-IDA protocol between 2007-2016, 36 of them female, with and average age of 53.4 years (DS+/-23.3). We treated with this protocol mostly patients with relapsed or refractory acute myeloid leukemia (RR-AML) (primary refractory or resistant AML as defined by not achieving complete remission after 1 cycle of intense induction therapy); 60% (n=38) of patients had a RR-AML, 37% (n=23) of them were relapsed AML and 23% (n=15) refractory AML. Based on European Prognostic Index Score (EPI-SCORE) for patients with RR-AML, 61% of them had a poor prognosis (10-14 points), 36% had an intermediate prognosis (7-9 points) and only 3% had a favorable prognosis (1-6 points). The next important group, 25% (n=17) were MDS patients transformed to AML. We had 9% (n=6) patients with treatment related AML and 6% with other acute leukemia (3 cases of refractory ALL and 1 case of biphenotypic leukemia).
Conclusion
Most AML patients ultimately die from their disease. In our case serie none died by any other cause. We had a similar response rate, mortality and overall survival that other groups in our country. Despite a variety of salvage therapy options, like FLAG-IDA protocol, prognosis in patients with RR-AML is generally poor and treatment is very complex.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): acute leukemia, Fludarabine, Ara-C (cytarabine)


