PREGNANCY ACCUMULATES UNFAVORABLE MOLECULAR GENETIC AML AND SHOULD BE CONSIDERED AS A POOR PROGNOSTIC FACTOR.
(Abstract release date: 05/18/17)
EHA Library. Troitskaya V. 05/18/17; 182399; PB1685

Vera Troitskaya
Contributions
Contributions
Abstract
Abstract: PB1685
Type: Publication Only
Background
Acute myeloid leukemia (AML) during pregnancy – is a rare clinical condition that limits the possibility to conduct large prospective clinical studies. All publications present small retrospective data and case reports. Most of them conclude that pregnancy doesn’t affect the prognosis of acute leukemia.
Aims
To assess the pregnancy, as independent prognostic factor, in non APL AML-patients (pts), prospectively treated within Russian AML multicenter studies.
Methods
From 1990 to 2017 yy the Russian Acute Leukemia study group has treated 33 with de novo AML pregnant women (Me-27 (21-42) yrs). AML was diagnosed in the Ist trimester in 1 woman (3%), in the IInd – 15 (45,5%), in the IIIrd - 17 (51,5%). Molecular genetic risk group was estimated in 27/33 pts: 52% (n=14) were referred to the intermediate risk group and 48% (n=13) to the poor prognosis. High risk group comprised complex karyotype (n=5), -7/del7 (n=4), translocations involving gene MLL (n=2), 1 pt - inv3/-7 and 1 pt - AML with myelodysplasia-related changes, normal karyotype and FLT-3+.
In 1 pt at the 1st trimester medical abortion was conducted and 11 women delivered at the gestation age of 34-40 weeks before chemotherapy (CT). 21 pregnant women received CT, that was started at 23 (14-32nd) weeks of gestation. Classical 7+3 was applied in all of pts: either with daunorubicin (45-60 mg/m2), or mitoxantrone (10 mg/m2), or idarubicin (12 mg/m2) regarding the treatment study-protocol.
Results
As our data show, AML in pregnancy is characterized by high prevalence of unfavorable cytogenetic abnormalities (48%), that is substantially different from AML in non-pregnant women of the same age (11,5%) (p=0,006) [Blood 2016,128;22,p.5171].
1 pt died before CT due to septic shock, 2 pts – in induction CT now. 2 pregnant women died due to severe infections in aplasia during induction (5,7%). So, induction results were evaluated in 30/33 pts: CR rate - 73,3% (22/30): after the 1st course CT - in 16 and after the 2nd – in 6 pts. In pts, with available cytogenetic data, CR was received in 100% (9/9) from the intermediate and in 80,0% (8/10) from the poor prognostic group. Primary resistance was registered in 6/30 pts (20%).
Antenatal fetal mortality was registered in 2 cases at the 21st and 32nd weeks during induction. 29 children were born.
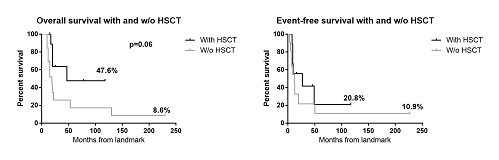
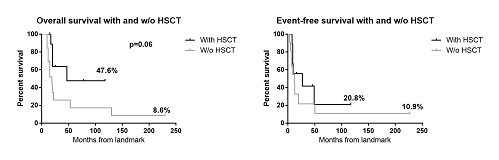
Allogenic bone marrow transplantation (allo-BMT) was done in 10 of 28 (35,7%) AML-pts who had survived induction therapy at a median of 6 months after CR. 4 pts relapsed after allo-BMT and 1 woman remained with refractory AML after allo-BMT. Our results demonstrated rather low 10-y OS and DFS (10,48% and 10,46%) in women, whom AML was diagnosed during pregnancy.
In order to evaluated the role of allo-BMT, we performed a landmark analysis (landmark=6 months of CR), that has shown better OS and DFS only in pts after allo-BMT (Pic).
Conclusion
Our results demonstrate: almost half of women, who were AML diagnosed during pregnancy, are referred to the poor molecular genetic prognostic group; they demonstrated very low OS and DFS whit their improvement after allo-BMT.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Prognostic factor, Pregnancy, Hematopoietic cell transplantation, Acute Myeloid Leukemia
Abstract: PB1685
Type: Publication Only
Background
Acute myeloid leukemia (AML) during pregnancy – is a rare clinical condition that limits the possibility to conduct large prospective clinical studies. All publications present small retrospective data and case reports. Most of them conclude that pregnancy doesn’t affect the prognosis of acute leukemia.
Aims
To assess the pregnancy, as independent prognostic factor, in non APL AML-patients (pts), prospectively treated within Russian AML multicenter studies.
Methods
From 1990 to 2017 yy the Russian Acute Leukemia study group has treated 33 with de novo AML pregnant women (Me-27 (21-42) yrs). AML was diagnosed in the Ist trimester in 1 woman (3%), in the IInd – 15 (45,5%), in the IIIrd - 17 (51,5%). Molecular genetic risk group was estimated in 27/33 pts: 52% (n=14) were referred to the intermediate risk group and 48% (n=13) to the poor prognosis. High risk group comprised complex karyotype (n=5), -7/del7 (n=4), translocations involving gene MLL (n=2), 1 pt - inv3/-7 and 1 pt - AML with myelodysplasia-related changes, normal karyotype and FLT-3+.
In 1 pt at the 1st trimester medical abortion was conducted and 11 women delivered at the gestation age of 34-40 weeks before chemotherapy (CT). 21 pregnant women received CT, that was started at 23 (14-32nd) weeks of gestation. Classical 7+3 was applied in all of pts: either with daunorubicin (45-60 mg/m2), or mitoxantrone (10 mg/m2), or idarubicin (12 mg/m2) regarding the treatment study-protocol.
Results
As our data show, AML in pregnancy is characterized by high prevalence of unfavorable cytogenetic abnormalities (48%), that is substantially different from AML in non-pregnant women of the same age (11,5%) (p=0,006) [Blood 2016,128;22,p.5171].
1 pt died before CT due to septic shock, 2 pts – in induction CT now. 2 pregnant women died due to severe infections in aplasia during induction (5,7%). So, induction results were evaluated in 30/33 pts: CR rate - 73,3% (22/30): after the 1st course CT - in 16 and after the 2nd – in 6 pts. In pts, with available cytogenetic data, CR was received in 100% (9/9) from the intermediate and in 80,0% (8/10) from the poor prognostic group. Primary resistance was registered in 6/30 pts (20%).
Antenatal fetal mortality was registered in 2 cases at the 21st and 32nd weeks during induction. 29 children were born.
Allogenic bone marrow transplantation (allo-BMT) was done in 10 of 28 (35,7%) AML-pts who had survived induction therapy at a median of 6 months after CR. 4 pts relapsed after allo-BMT and 1 woman remained with refractory AML after allo-BMT. Our results demonstrated rather low 10-y OS and DFS (10,48% and 10,46%) in women, whom AML was diagnosed during pregnancy.
In order to evaluated the role of allo-BMT, we performed a landmark analysis (landmark=6 months of CR), that has shown better OS and DFS only in pts after allo-BMT (Pic).
Conclusion
Our results demonstrate: almost half of women, who were AML diagnosed during pregnancy, are referred to the poor molecular genetic prognostic group; they demonstrated very low OS and DFS whit their improvement after allo-BMT.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Prognostic factor, Pregnancy, Hematopoietic cell transplantation, Acute Myeloid Leukemia
{{ help_message }}
{{filter}}


