
Contributions
Abstract: S806
Type: Oral Presentation
Presentation during EHA22: On Sunday, June 25, 2017 from 08:30 - 08:45
Location: Room N104
Background
Infection-related mortality (IRM) is a major challenge after allogeneic hematopoietic stem cell transplantation (allo-HSCT).
Aims
The aim of this study was to develop a scoring system predicting IRM based exclusively on pre-transplant data.
Methods
A total of 589 adult patients receiving allo-HSCT were studied (Jan 2009 - Nov 2016). In a training set of patients (n=273, Jan 2012-May 2015) the ROC curve analysis defined the optimal cut-offs predicting 100-day IRM for continuous data. All clinical and biochemical variables were challenged in a multivariate analysis and a 3-tiered weighted score was elaborated and tested firstly in a retrospective validation set (n=219, Jan 2009-Dec 2011) and then in a prospective validation set (n=97, Jun 2016-Nov 2016).
Results
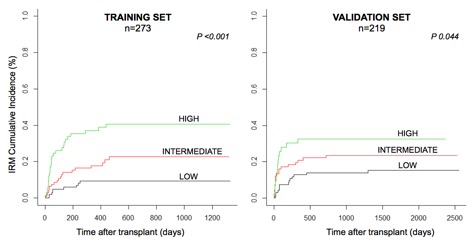
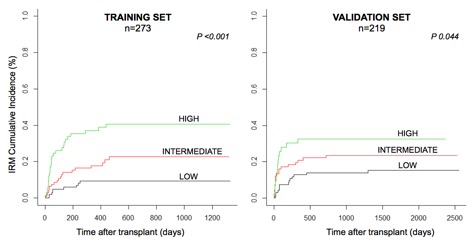
Median follow-up was 43 months (range 1-85). Acute leukemia was the main indication to transplant, accounting for 60% (n=356) of patients. The majority of the patients received an alternative-donor transplant (44% a HLA-haploidentical, 37% a matched unrelated donor). Forty-seven percent (n=277) of patients had advanced diseases. Multivariate analysis revealed age >60 yrs (P=0.003), CMV host/donor serostatus different from negative/negative (P<0.001) and pre-transplant levels of IgA <1.11 g/L (P=0.004) and IgM <0.305 g/L (P=0.028) as the only independent predictors of increased IRM. Noticeably, these associations were independent from disease type or status, donor type, intensity of conditioning, in vivo T or B-cell depletion or from previous colonization by multidrug-resistant bacteria. According to the proposed IRM score, patients were divided into 3 classes: low (<10.17 points), intermediate (10.17-11.11 points) or high-risk (>11.11 points). In the training set, 100-day and 2-yrs IRM were 5% (95% CI 2-10) and 9% (95% CI 4-16) for low-risk, 11% (95% CI 5-18) and 23% (95% CI 14-33) for intermediate-risk, and 16% (95% CI 16-37) and 41% (95% CI 28-53) for high-risk patients, respectively (P=0.001). In the retrospective validation set, 100-day and 2-yrs IRM were 7% (95% CI 3-14) and 14% (95% CI 8-22) for low-risk, 17% (95% CI 10-26) and 23% (95% CI 15-33) for intermediate, and 28% (95% CI 15-42) and 33% (95% CI 19-4) for high-risk patients, respectively (P= 0.044), with a c-index of 0.608 (Figure 1). In the prospective validation set, only 100-day IRM was calculated due to a shorter follow-up, being of 0%, 3% (95% CI 0-13) and of 14% (95% CI 3-33) for low, intermediate and high-risk patients (P=0.003). Additionally, in both training and retrospective validation sets (n=492), the 2-yrs OS was different among the 3 groups, being 59% (95%CI 52-67), 50% (95%CI 43-59) and 37% (95%CI 29-48) for low, intermediate and high-risk groups, respectively (P=0.0001). In the prospective validation set, only 100-day OS was evaluated, being of 95% (95%CI 88-100), 91% (95%CI 82-100) and 80% (95%CI 65-100), respectively (P=0.03). Out of a total of 129 infection-related deaths, 94/129 (73%) were attributed to bacteria, 22/129 (17%) to viruses, 11/129 (8%) to fungi and 2/129 8 (2%) to parasites.
Conclusion
This new clinic-biological score based on age, CMV serostatus and levels of IgA and IgM, may contribute to the prompt identification of patients at higher risk of fatal infections prior to allo-HSCT, thus promoting post-transplant personalized intensive active surveillance strategies and immune-intervention approaches to improve the overall outcome of transplant. A multicentric Italian study in currently on the way for the external validation of these results
Session topic: 29. Infectious diseases, supportive care
Keyword(s): Allogeneic hematopoietic stem cell transplant, Prognostic factor, Infection, Immunoglobulin
Abstract: S806
Type: Oral Presentation
Presentation during EHA22: On Sunday, June 25, 2017 from 08:30 - 08:45
Location: Room N104
Background
Infection-related mortality (IRM) is a major challenge after allogeneic hematopoietic stem cell transplantation (allo-HSCT).
Aims
The aim of this study was to develop a scoring system predicting IRM based exclusively on pre-transplant data.
Methods
A total of 589 adult patients receiving allo-HSCT were studied (Jan 2009 - Nov 2016). In a training set of patients (n=273, Jan 2012-May 2015) the ROC curve analysis defined the optimal cut-offs predicting 100-day IRM for continuous data. All clinical and biochemical variables were challenged in a multivariate analysis and a 3-tiered weighted score was elaborated and tested firstly in a retrospective validation set (n=219, Jan 2009-Dec 2011) and then in a prospective validation set (n=97, Jun 2016-Nov 2016).
Results
Median follow-up was 43 months (range 1-85). Acute leukemia was the main indication to transplant, accounting for 60% (n=356) of patients. The majority of the patients received an alternative-donor transplant (44% a HLA-haploidentical, 37% a matched unrelated donor). Forty-seven percent (n=277) of patients had advanced diseases. Multivariate analysis revealed age >60 yrs (P=0.003), CMV host/donor serostatus different from negative/negative (P<0.001) and pre-transplant levels of IgA <1.11 g/L (P=0.004) and IgM <0.305 g/L (P=0.028) as the only independent predictors of increased IRM. Noticeably, these associations were independent from disease type or status, donor type, intensity of conditioning, in vivo T or B-cell depletion or from previous colonization by multidrug-resistant bacteria. According to the proposed IRM score, patients were divided into 3 classes: low (<10.17 points), intermediate (10.17-11.11 points) or high-risk (>11.11 points). In the training set, 100-day and 2-yrs IRM were 5% (95% CI 2-10) and 9% (95% CI 4-16) for low-risk, 11% (95% CI 5-18) and 23% (95% CI 14-33) for intermediate-risk, and 16% (95% CI 16-37) and 41% (95% CI 28-53) for high-risk patients, respectively (P=0.001). In the retrospective validation set, 100-day and 2-yrs IRM were 7% (95% CI 3-14) and 14% (95% CI 8-22) for low-risk, 17% (95% CI 10-26) and 23% (95% CI 15-33) for intermediate, and 28% (95% CI 15-42) and 33% (95% CI 19-4) for high-risk patients, respectively (P= 0.044), with a c-index of 0.608 (Figure 1). In the prospective validation set, only 100-day IRM was calculated due to a shorter follow-up, being of 0%, 3% (95% CI 0-13) and of 14% (95% CI 3-33) for low, intermediate and high-risk patients (P=0.003). Additionally, in both training and retrospective validation sets (n=492), the 2-yrs OS was different among the 3 groups, being 59% (95%CI 52-67), 50% (95%CI 43-59) and 37% (95%CI 29-48) for low, intermediate and high-risk groups, respectively (P=0.0001). In the prospective validation set, only 100-day OS was evaluated, being of 95% (95%CI 88-100), 91% (95%CI 82-100) and 80% (95%CI 65-100), respectively (P=0.03). Out of a total of 129 infection-related deaths, 94/129 (73%) were attributed to bacteria, 22/129 (17%) to viruses, 11/129 (8%) to fungi and 2/129 8 (2%) to parasites.
Conclusion
This new clinic-biological score based on age, CMV serostatus and levels of IgA and IgM, may contribute to the prompt identification of patients at higher risk of fatal infections prior to allo-HSCT, thus promoting post-transplant personalized intensive active surveillance strategies and immune-intervention approaches to improve the overall outcome of transplant. A multicentric Italian study in currently on the way for the external validation of these results
Session topic: 29. Infectious diseases, supportive care
Keyword(s): Allogeneic hematopoietic stem cell transplant, Prognostic factor, Infection, Immunoglobulin


