ALLOGENEIC STEM CELL TRANSPLANTATION FOR ACUTE MYELOID LEUKEMIA WITH DELETION 5Q OR MONOSOMY 5: A STUDY FROM THE ACUTE LEUKEMIA WORKING PARTY (ALWP) OF THE EBMT
(Abstract release date: 05/18/17)
EHA Library. Poiré X. 06/25/17; 182085; S798

Xavier Poiré
Contributions
Contributions
Abstract
Abstract: S798
Type: Oral Presentation
Presentation during EHA22: On Sunday, June 25, 2017 from 09:00 - 09:15
Location: Room N105
Background
High-risk acute myeloid leukemia (AML) is mainly defined by the presence of determined poor-risk cytogenetic abnormalities and is a standard indication for allogenetic stem cell transplantation (SCT). Nevertheless, high-risk AML is a very heterogeneous group including several abnormalities with different levels of prognostic impact. Deletion 5q or monosomy 5 (-5/5q-) has been part of the high-risk group of AML for many years. SCT seems to improve their outcomes but the additive effects of other high-risk cytogenetic features on survival have never been thoroughly studied.
Aims
To evaluate the role of SCT in -5/5q- AML with additional cytogenetic abnormalities such as complex karyotype (CK), monosomal karyotype (MK), monosomy 7 (-7), or 17p abnormalities (abn(17p)).
Methods
We included adult patients (pts) with AML with -5/5q- reported to the EBMT registry as having their first SCT between 2000 and 2015.
Results
Five hundred and one pts, 21% of them with secondary AML, have been allocated. Median age at SCT was 55 year-old (range, 18-75) and median follow-up was 21 months (range, 2-173). At time of SCT, 338 pts (67%) were in first remission (CR1), 21 pts (4%) were in subsequent remission and 142 (28%) had active disease. Two hundred seventy-seven pts (55%) were transplanted from an unrelated donor (UD) and 224 from a sibling donor. A myeloablative conditioning (MAC) was administered in 45% of the pts and a reduced-intensity conditioning (RIC) in 55% of them.
The 2-year probabilities of overall survival (OS) and leukemia-free survival (LFS) were 27% and 20%, respectively. The 2-year probality of treatment-related mortality (TRM) was 20%. The cumulative incidence of grade II-IV acute graft-versus-host disease (GvHD) was 29% and the 2-year cumulative incidence of chronic GvHD was 27%. The main cause of death was disease-related. In multivariate analysis, active disease correlated strongly with worse OS, LFS and NRM. The other factors influencing outcomes were UD with increased NRM, and age with decreased OS and LFS.
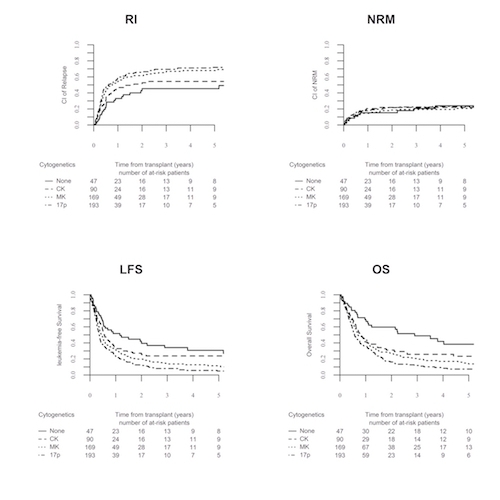
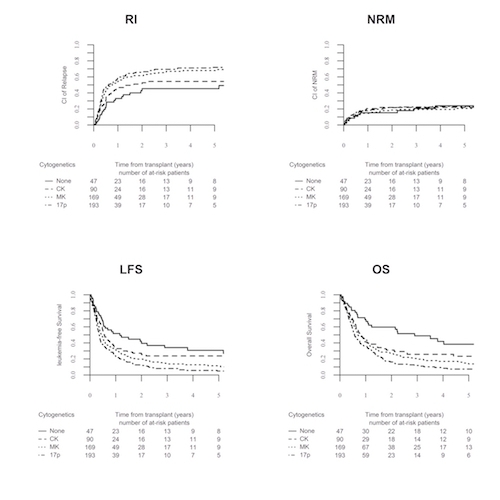
Based on the frequencies of the different additional cytogenetic abnormalities, we identified 4 groups within our cohort. Group 1 (None) included 47 pts with -5/5q- but without CK, MK or abn(17p). Group 2 (CK) included pts with -5/5q- and CK but no MK or abn(17p) (N=90). Group 3 (MK) included 169 pts with -5/5q- and MK but no abn(17p). Finally, group 4 (17p) included pts with -5/5q- and abn(17p) (N=193). The 4 groups were quite similar in term of characteristics. The 2-year probablity of LFS was 39% for group 1, 25% for group 2, 20% for group 3 and only 13% for group 4 (p<0.001). OS decreased also significantly from group 1 to group 4 (p<0.001). NRM was similar across the groups. In multivariate analysis, factors associated with worse OS and LFS were active disease, age, MK and abn(17p). The corresponding 2-year probability of GvHD and relapse-free survival was 27% for group 1, 17% for group 2, 14% for group 3 and 7% for group 4.
Conclusion
SCT in -5/5q- AML provides a durable response for approximately 20% of pts. Active disease at time of transplantation was the most powerful predictor of an inferior outcome. The presence of -5/5q- without CK, MK or abn(17p) was associated with a significant better survival and the addition of MK or abn(17p) translated into worse outcomes. We confirmed the deleterious effect of the combination of -5/5q- and abn(17p) on SCT outcome. Future efforts should be focused on this subgroup in order to improve their outcome.
Session topic: 22. Stem cell transplantation - Clinical
Keyword(s): Cytogenetics, Allogeneic hematopoietic stem cell transplant, Acute Myeloid Leukemia
Abstract: S798
Type: Oral Presentation
Presentation during EHA22: On Sunday, June 25, 2017 from 09:00 - 09:15
Location: Room N105
Background
High-risk acute myeloid leukemia (AML) is mainly defined by the presence of determined poor-risk cytogenetic abnormalities and is a standard indication for allogenetic stem cell transplantation (SCT). Nevertheless, high-risk AML is a very heterogeneous group including several abnormalities with different levels of prognostic impact. Deletion 5q or monosomy 5 (-5/5q-) has been part of the high-risk group of AML for many years. SCT seems to improve their outcomes but the additive effects of other high-risk cytogenetic features on survival have never been thoroughly studied.
Aims
To evaluate the role of SCT in -5/5q- AML with additional cytogenetic abnormalities such as complex karyotype (CK), monosomal karyotype (MK), monosomy 7 (-7), or 17p abnormalities (abn(17p)).
Methods
We included adult patients (pts) with AML with -5/5q- reported to the EBMT registry as having their first SCT between 2000 and 2015.
Results
Five hundred and one pts, 21% of them with secondary AML, have been allocated. Median age at SCT was 55 year-old (range, 18-75) and median follow-up was 21 months (range, 2-173). At time of SCT, 338 pts (67%) were in first remission (CR1), 21 pts (4%) were in subsequent remission and 142 (28%) had active disease. Two hundred seventy-seven pts (55%) were transplanted from an unrelated donor (UD) and 224 from a sibling donor. A myeloablative conditioning (MAC) was administered in 45% of the pts and a reduced-intensity conditioning (RIC) in 55% of them.
The 2-year probabilities of overall survival (OS) and leukemia-free survival (LFS) were 27% and 20%, respectively. The 2-year probality of treatment-related mortality (TRM) was 20%. The cumulative incidence of grade II-IV acute graft-versus-host disease (GvHD) was 29% and the 2-year cumulative incidence of chronic GvHD was 27%. The main cause of death was disease-related. In multivariate analysis, active disease correlated strongly with worse OS, LFS and NRM. The other factors influencing outcomes were UD with increased NRM, and age with decreased OS and LFS.
Based on the frequencies of the different additional cytogenetic abnormalities, we identified 4 groups within our cohort. Group 1 (None) included 47 pts with -5/5q- but without CK, MK or abn(17p). Group 2 (CK) included pts with -5/5q- and CK but no MK or abn(17p) (N=90). Group 3 (MK) included 169 pts with -5/5q- and MK but no abn(17p). Finally, group 4 (17p) included pts with -5/5q- and abn(17p) (N=193). The 4 groups were quite similar in term of characteristics. The 2-year probablity of LFS was 39% for group 1, 25% for group 2, 20% for group 3 and only 13% for group 4 (p<0.001). OS decreased also significantly from group 1 to group 4 (p<0.001). NRM was similar across the groups. In multivariate analysis, factors associated with worse OS and LFS were active disease, age, MK and abn(17p). The corresponding 2-year probability of GvHD and relapse-free survival was 27% for group 1, 17% for group 2, 14% for group 3 and 7% for group 4.
Conclusion
SCT in -5/5q- AML provides a durable response for approximately 20% of pts. Active disease at time of transplantation was the most powerful predictor of an inferior outcome. The presence of -5/5q- without CK, MK or abn(17p) was associated with a significant better survival and the addition of MK or abn(17p) translated into worse outcomes. We confirmed the deleterious effect of the combination of -5/5q- and abn(17p) on SCT outcome. Future efforts should be focused on this subgroup in order to improve their outcome.
Session topic: 22. Stem cell transplantation - Clinical
Keyword(s): Cytogenetics, Allogeneic hematopoietic stem cell transplant, Acute Myeloid Leukemia
{{ help_message }}
{{filter}}


