IS FCR THE TREATMENT OF CHOICE FOR IGHV MUTATED CLL WITHOUT POOR FISH CYTOGENETICS?
(Abstract release date: 05/18/17)
EHA Library. Cuellar c. 06/24/17; 181749; S462

carolina Cuellar
Contributions
Contributions
Abstract
Abstract: S462
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 16:15 - 16:30
Location: Hall B
Background
Chemoimmunotherapy (CIT) is the standard treatment for young and fit treatment-naïve patients with CLL. The median progression-free-survival (PFS) in patients treated with CIT is about 5-6 years and the overall survival (OS) is increased by 5-10% compared to those treated with chemotherapy only. Patients with mutated IGHV genes (M-CLL) and no unfavorable cytogenetic alterations (i.e. del(17p)/TP53 mutation, and del(11q)) have a better outcome than those with unmutated IGHV genes (U-CLL) and/or poor FISH cytogenetics and show a plateau in survival curves, suggesting that a fraction of these patients may have a survival similar to general population. Nevertheless, the possibility that some M-CLL patients without unfavorable cytogenetics are overtreated is of concern because of the treatment toxicity related to CIT, particularly FCR.
Aims
The aim of this study was to analyse the outcome of M-CLL patients with no unfavorable cytogenetics CLL according to the type of therapy.
Methods
We analysed 816 CLL patients from Sant Pau Hospital, Barcelona, Spain; Uppsala Universitary Hospital, Sweden and IRCCS San Raffaele Scientific University, Milan, Italy for whom IGHV mutational status was available. Endpoints were OS and TFS.
Results
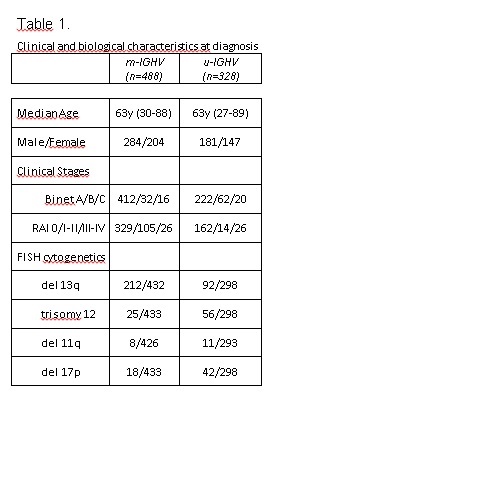
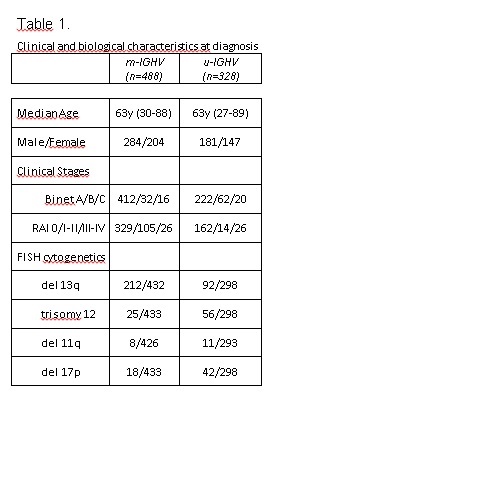
488 patients had mutated IGHV genes (400 without unfavorable FISH cytogenetics; 26 had either del(11q) and/or del(17p), and in 62 cases FISH was not available) and 328 patients carried unmutated IGHV genes. The main clinical and biological characteristics at diagnosis are shown in Table 1. OS at 5 and 10 years was 93% (CI, 95-91) and 81% (CI, 85-77) for M-CLL cases and 78% (CI, 83-73) and 46% (CI, 52-39) for U-CLL cases (p<0.05). TFS at 5 and 10 years was 73% (CI, 77-69) and 61% (CI, 66-56) and 28% (CI, 33-23) and 10% (CI, 14-6) for M-CLL and U-CLL, respectively (p<0.05). After a median follow-up of 8 years (range, 1-26), 424 patients [161 M-CLL (136 without poor-prognostic FISH cytogenetics, 13 with either del(11q) and/or del(17p) and 12 cases in whom FISH information was not available) and 263 U-CLL] required therapy. Front-line treatment consisted of purine analogues (PA)-based therapy (n=83), alkylating agents (n=212), anti-CD20 moAbs with PA or bendamustine (n=75), anti-CD20 moAbs with alkylating agents (n=21), BCR-signal inhibitors or BCL2 antiapoptotic agents (n=9), others (n=23), and unknown (n=1). The median duration of response to first therapy was 42 months (range, 33-52) in M-CLL cases vs 24 months (range, 18-30) in U-CLL patients (p<0.001). 282 patients received a second line of therapy: PA-based therapy (n=95), alkylating agents (n=82), anti-CD20 moAbs with PA or bendamustine (n=33), anti-CD20 moAbs with alkylating agents (n=16), BCR-signal inhibitors or BCL2 antiapoptotic agents (n=12), others (n=39), and unknown (n=5). In 481 of 816 patients in whom detailed information on treatment regimens beyond second-line was available, 99 patients received a third-line treatment including PA-based therapy (n=15), alkylating regimens (n=20), anti-CD20 MoAbs with PA or bendamustine (n=15), anti-CD20 moAbs with alkylating agents (n=8), BCR or BCL2 inhibitors (n=11), others (n=28) and unknown (n=2); 49 patients received four or more lines of therapy. In M-CLL patients without poor FISH cytogenetics (n=136) the type of therapy did not impact patients´ outcome. Thus, the median survival was not reached in patients treated with CIT as first-line (i.e FCR, BR) as compared to 202 months in those not having received CIT (p=0.317). In contrast, in U-CLL patients the OS was highly dependent on the type of therapy. In detail, U-CLL patients who received anti-CD20 MoAbs with PA or bendamustine either as first line or subsequent lines (60 of 120 patients) showed significantly longer survival than those who did not receive these therapeutic regimens (median survival: 173 vs 103 months, p=0.001). On the contrary, in M-CLL cases no differences in survival were observed in those receiving anti-CD20 MoAbs with PA or bendamustine vs who did not (p= 0.558).
Conclusion
This retrospective study suggests that OS of CLL patients with mutated IGHV genes and no unfavorable FISH cytogenetics do not depend on the type of therapy. This has important clinical implications and provides background for randomized studies aimed at identifying the optimal treatment strategy for this group of patients.
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): Chronic Lymphocytic Leukemia, Mutation status, Immunotherapy
Abstract: S462
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 16:15 - 16:30
Location: Hall B
Background
Chemoimmunotherapy (CIT) is the standard treatment for young and fit treatment-naïve patients with CLL. The median progression-free-survival (PFS) in patients treated with CIT is about 5-6 years and the overall survival (OS) is increased by 5-10% compared to those treated with chemotherapy only. Patients with mutated IGHV genes (M-CLL) and no unfavorable cytogenetic alterations (i.e. del(17p)/TP53 mutation, and del(11q)) have a better outcome than those with unmutated IGHV genes (U-CLL) and/or poor FISH cytogenetics and show a plateau in survival curves, suggesting that a fraction of these patients may have a survival similar to general population. Nevertheless, the possibility that some M-CLL patients without unfavorable cytogenetics are overtreated is of concern because of the treatment toxicity related to CIT, particularly FCR.
Aims
The aim of this study was to analyse the outcome of M-CLL patients with no unfavorable cytogenetics CLL according to the type of therapy.
Methods
We analysed 816 CLL patients from Sant Pau Hospital, Barcelona, Spain; Uppsala Universitary Hospital, Sweden and IRCCS San Raffaele Scientific University, Milan, Italy for whom IGHV mutational status was available. Endpoints were OS and TFS.
Results
488 patients had mutated IGHV genes (400 without unfavorable FISH cytogenetics; 26 had either del(11q) and/or del(17p), and in 62 cases FISH was not available) and 328 patients carried unmutated IGHV genes. The main clinical and biological characteristics at diagnosis are shown in Table 1. OS at 5 and 10 years was 93% (CI, 95-91) and 81% (CI, 85-77) for M-CLL cases and 78% (CI, 83-73) and 46% (CI, 52-39) for U-CLL cases (p<0.05). TFS at 5 and 10 years was 73% (CI, 77-69) and 61% (CI, 66-56) and 28% (CI, 33-23) and 10% (CI, 14-6) for M-CLL and U-CLL, respectively (p<0.05). After a median follow-up of 8 years (range, 1-26), 424 patients [161 M-CLL (136 without poor-prognostic FISH cytogenetics, 13 with either del(11q) and/or del(17p) and 12 cases in whom FISH information was not available) and 263 U-CLL] required therapy. Front-line treatment consisted of purine analogues (PA)-based therapy (n=83), alkylating agents (n=212), anti-CD20 moAbs with PA or bendamustine (n=75), anti-CD20 moAbs with alkylating agents (n=21), BCR-signal inhibitors or BCL2 antiapoptotic agents (n=9), others (n=23), and unknown (n=1). The median duration of response to first therapy was 42 months (range, 33-52) in M-CLL cases vs 24 months (range, 18-30) in U-CLL patients (p<0.001). 282 patients received a second line of therapy: PA-based therapy (n=95), alkylating agents (n=82), anti-CD20 moAbs with PA or bendamustine (n=33), anti-CD20 moAbs with alkylating agents (n=16), BCR-signal inhibitors or BCL2 antiapoptotic agents (n=12), others (n=39), and unknown (n=5). In 481 of 816 patients in whom detailed information on treatment regimens beyond second-line was available, 99 patients received a third-line treatment including PA-based therapy (n=15), alkylating regimens (n=20), anti-CD20 MoAbs with PA or bendamustine (n=15), anti-CD20 moAbs with alkylating agents (n=8), BCR or BCL2 inhibitors (n=11), others (n=28) and unknown (n=2); 49 patients received four or more lines of therapy. In M-CLL patients without poor FISH cytogenetics (n=136) the type of therapy did not impact patients´ outcome. Thus, the median survival was not reached in patients treated with CIT as first-line (i.e FCR, BR) as compared to 202 months in those not having received CIT (p=0.317). In contrast, in U-CLL patients the OS was highly dependent on the type of therapy. In detail, U-CLL patients who received anti-CD20 MoAbs with PA or bendamustine either as first line or subsequent lines (60 of 120 patients) showed significantly longer survival than those who did not receive these therapeutic regimens (median survival: 173 vs 103 months, p=0.001). On the contrary, in M-CLL cases no differences in survival were observed in those receiving anti-CD20 MoAbs with PA or bendamustine vs who did not (p= 0.558).
Conclusion
This retrospective study suggests that OS of CLL patients with mutated IGHV genes and no unfavorable FISH cytogenetics do not depend on the type of therapy. This has important clinical implications and provides background for randomized studies aimed at identifying the optimal treatment strategy for this group of patients.
Session topic: 6. Chronic lymphocytic leukemia and related disorders - Clinical
Keyword(s): Chronic Lymphocytic Leukemia, Mutation status, Immunotherapy
{{ help_message }}
{{filter}}


