
Contributions
Abstract: S450
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 12:30 - 12:45
Location: Room N104
Background
Aberrant B-cell homeostasis has been described in patients (pts) with chronic graft-versus-host disease (cGVHD) following allogeneic stem cell transplantation (allo-SCT). However, there is no information on the predictive value of specific B-cell subsets of the incidence of cGVHD.
Aims
We sought to determine if B-cell subsets measured around day 100 after allo-SCT predict the subsequent occurrence of cGVHD in a prospective clinical study.
Methods
Peripheral blood (PB) samples were obtained from consented patients (pts) between day 80 and 110 (D100) after allo-SCT at The University of Texas MD Anderson Cancer Center from 2012 to 2015. Only pts who had not been diagnosed with cGVHD or progression of underlying malignancy by D100 were eligible for this study. We analyzed CD19+CD20+ B cell subsets by FACS. Subsets were defined as naïve (CD27-IgD+), unswitched (CD27+IgD+) and switched (CD27+IgD-) memory cells. Receiver Operating Characteristic (ROC) curve was used to identify threshold levels of B cell % and numbers that predict the incidence of cGVHD. cGVHD diagnosis was based on the 2014 National Institutes of Health guidelines.
Results
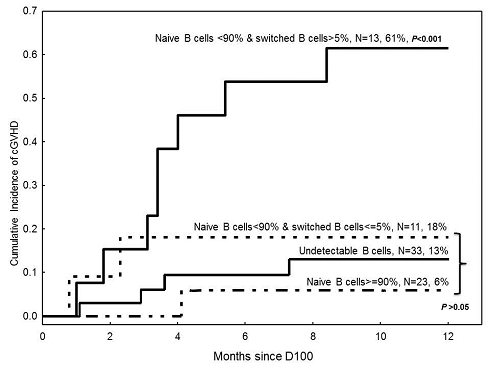
A total of 80 pts were enrolled in the study. The median age at SCT was 49 years (range 21-75). The majority (80%) of pts received myeloablative conditioning, and 75% received tacrolimus with methotrexate or mycophenolate mofetil for GVHD prophylaxis. Diagnosis was myeloid (61%) or lymphoid (34%) malignancy in the majority of pts. Grafts source was primarily PB or bone marrow from matched- unrelated (61%) or related (24%) donors. Grade 2-4 acute GVHD had occurred in 45% of pts before D100. Thirty-six percent of pts were receiving steroids at D100. Forty-seven (59%) pts had detectable (≥ 0.1%) CD19+CD20+ signal on D100. In this subset, median B cell % was 3 (range 0.25-34) and median absolute number was 23 (1.8-419) x103 cells /µL. Median % naïve, unswitched, and switched B cells was 89% (54-99), 1.85% (0.3-8.5), and 2.1% (0-30), respectively. A total of 15 pts were diagnosed with cGVHD within 1 year after D100 including 11 with detectable B cells. ROC analysis did not identify predictive thresholds for overall B cell % or numbers. However, it identified predictive thresholds for each of the B cell subsets analyzed. The area under the curve (AUC) analysis indicated that % naïve (cutoff 87.3%) and % switched (cutoff 4%) B cells were the most significant (AUC 86%) predictors of the incidence of cGVHD. Rounding up the cutoff values, we grouped pts into 3 mutually exclusive groups: 1) naïve B cells ≥90% (n=23, none had >5% switched B cells), 2) naïve B cells <90% and switched B cells ≤5% (n=11), and 3) naïve B cells <90% and switched B cells >5% (n=13). Patients (n=33) with undetectable B cells were considered together as one group. The rate of cGVHD after D100 was significantly higher in pts with <90% naïve and >5% switched B cells (HR=7, p<0.001) with a 1-year cumulative incidence of 61% (Figure). None of the characteristics listed above were significantly associated with the rate of cGVHD. Percent naive and switched B cells did not correlate with receipt of steroids on D100. Patients with undetectable B cells were significantly more likely to have an underlying lymphoid vs. myeloid malignancy (58% vs. 33%, p< 0.001); and those with ≥90% naïve B cells were significantly more likely to be ≤55 years of age at the time of allo-SCT (83% vs 42%, p=0.004).
Conclusion
In conclusion, D100 frequency of naïve and switched B cells predicts the subsequent development of cGVHD. Lymphoid malignancies and older age may be associated with aberrant B-cell reconstitution. Consideration of D100 B-cell subsets may improve risk stratification models for the development of cGVHD.
Session topic: 22. Stem cell transplantation - Clinical
Keyword(s): Graft-versus-host disease (GVHD), B cell subsets, Allo-SCT
Abstract: S450
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 12:30 - 12:45
Location: Room N104
Background
Aberrant B-cell homeostasis has been described in patients (pts) with chronic graft-versus-host disease (cGVHD) following allogeneic stem cell transplantation (allo-SCT). However, there is no information on the predictive value of specific B-cell subsets of the incidence of cGVHD.
Aims
We sought to determine if B-cell subsets measured around day 100 after allo-SCT predict the subsequent occurrence of cGVHD in a prospective clinical study.
Methods
Peripheral blood (PB) samples were obtained from consented patients (pts) between day 80 and 110 (D100) after allo-SCT at The University of Texas MD Anderson Cancer Center from 2012 to 2015. Only pts who had not been diagnosed with cGVHD or progression of underlying malignancy by D100 were eligible for this study. We analyzed CD19+CD20+ B cell subsets by FACS. Subsets were defined as naïve (CD27-IgD+), unswitched (CD27+IgD+) and switched (CD27+IgD-) memory cells. Receiver Operating Characteristic (ROC) curve was used to identify threshold levels of B cell % and numbers that predict the incidence of cGVHD. cGVHD diagnosis was based on the 2014 National Institutes of Health guidelines.
Results
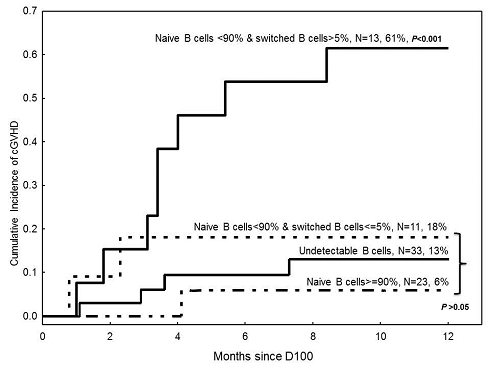
A total of 80 pts were enrolled in the study. The median age at SCT was 49 years (range 21-75). The majority (80%) of pts received myeloablative conditioning, and 75% received tacrolimus with methotrexate or mycophenolate mofetil for GVHD prophylaxis. Diagnosis was myeloid (61%) or lymphoid (34%) malignancy in the majority of pts. Grafts source was primarily PB or bone marrow from matched- unrelated (61%) or related (24%) donors. Grade 2-4 acute GVHD had occurred in 45% of pts before D100. Thirty-six percent of pts were receiving steroids at D100. Forty-seven (59%) pts had detectable (≥ 0.1%) CD19+CD20+ signal on D100. In this subset, median B cell % was 3 (range 0.25-34) and median absolute number was 23 (1.8-419) x103 cells /µL. Median % naïve, unswitched, and switched B cells was 89% (54-99), 1.85% (0.3-8.5), and 2.1% (0-30), respectively. A total of 15 pts were diagnosed with cGVHD within 1 year after D100 including 11 with detectable B cells. ROC analysis did not identify predictive thresholds for overall B cell % or numbers. However, it identified predictive thresholds for each of the B cell subsets analyzed. The area under the curve (AUC) analysis indicated that % naïve (cutoff 87.3%) and % switched (cutoff 4%) B cells were the most significant (AUC 86%) predictors of the incidence of cGVHD. Rounding up the cutoff values, we grouped pts into 3 mutually exclusive groups: 1) naïve B cells ≥90% (n=23, none had >5% switched B cells), 2) naïve B cells <90% and switched B cells ≤5% (n=11), and 3) naïve B cells <90% and switched B cells >5% (n=13). Patients (n=33) with undetectable B cells were considered together as one group. The rate of cGVHD after D100 was significantly higher in pts with <90% naïve and >5% switched B cells (HR=7, p<0.001) with a 1-year cumulative incidence of 61% (Figure). None of the characteristics listed above were significantly associated with the rate of cGVHD. Percent naive and switched B cells did not correlate with receipt of steroids on D100. Patients with undetectable B cells were significantly more likely to have an underlying lymphoid vs. myeloid malignancy (58% vs. 33%, p< 0.001); and those with ≥90% naïve B cells were significantly more likely to be ≤55 years of age at the time of allo-SCT (83% vs 42%, p=0.004).
Conclusion
In conclusion, D100 frequency of naïve and switched B cells predicts the subsequent development of cGVHD. Lymphoid malignancies and older age may be associated with aberrant B-cell reconstitution. Consideration of D100 B-cell subsets may improve risk stratification models for the development of cGVHD.
Session topic: 22. Stem cell transplantation - Clinical
Keyword(s): Graft-versus-host disease (GVHD), B cell subsets, Allo-SCT


