
Contributions
Abstract: S444
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 12:15 - 12:30
Location: Room N103
Background
Aims
To evaluate the impact of a new version (v2.0) of our e-alert system for VTE prevention compared with the initial software version. Secondary endpoints try to identify predictive factors for prophylaxis use and thrombotic events.
Methods
Prospective study including consecutive adult cancer patients admitted at our centre. From April 2014 to June 2015 (first period) the initial e-alert system version remained operative and from July 2015 to December 2016 (second period) the new version was active. The v2.0 displayed a second window that asked physicians about the reason why LMHW was not prescribed. The main outcomes were: VTE (confirmed by objective methods), clinically relevant bleeding, and mortality. All patients were followed-up during hospitalisation and 30 days after discharge. Descriptive statistical analysis and correlation between clinical variables and main outcomes were performed by using the software package SSPS v20.
Results
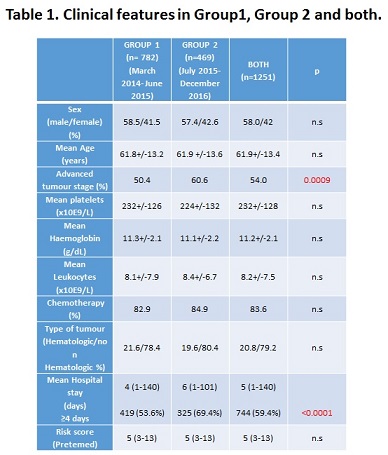
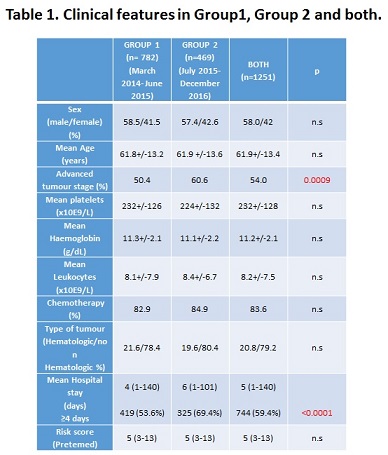
1251 patients were included, 782 patients in the first period and 469 in the second one (main clinical features are shown in Table 1). E-alerts v2.0 was associated with an increase of appropriate LMWH prophylaxis during hospitalisation (65.2% vs 72.2%; p=0.015). However, this improvement did not result in a reduction of VTE during admission or follow-up (2.3% vs 2.3%; p=0.89). Interestingly, almost 80% of VTE events occurred despite LMWH use. No differences in the rate of major bleeding (2.8% vs 3.2%; p=0.83), and mortality (10.6% vs 14.3%; p=0.07) were observed, either. The main reason for not prescribing LMWH prophylaxis was bleeding risk, but in 17% of cases physicians did not consider that the patient really had a high VTE risk. No significant correlation was found between any of the clinical variables analyzed and the risk of VTE. Prophylaxis use was more frequent among patients with solid cancer (vs hematologic), advanced stage, active chemotherapy treatment and longer hospital stay.
Conclusion
The new e-alert system further increases the use of VTE prophylaxis in hospitalised cancer patients, although this was not associated with a reduction in the VTE incidence. A relevant number of VTE events occur despite prophylaxis with standard LMWH. Identificaton of risk factors for thromboprophylaxis failure is needed.
Session topic: 34. Thrombosis and vascular biology
Keyword(s): Venous thromboembolism, Thromboprophylaxis, Cancer
Abstract: S444
Type: Oral Presentation
Presentation during EHA22: On Saturday, June 24, 2017 from 12:15 - 12:30
Location: Room N103
Background
Aims
To evaluate the impact of a new version (v2.0) of our e-alert system for VTE prevention compared with the initial software version. Secondary endpoints try to identify predictive factors for prophylaxis use and thrombotic events.
Methods
Prospective study including consecutive adult cancer patients admitted at our centre. From April 2014 to June 2015 (first period) the initial e-alert system version remained operative and from July 2015 to December 2016 (second period) the new version was active. The v2.0 displayed a second window that asked physicians about the reason why LMHW was not prescribed. The main outcomes were: VTE (confirmed by objective methods), clinically relevant bleeding, and mortality. All patients were followed-up during hospitalisation and 30 days after discharge. Descriptive statistical analysis and correlation between clinical variables and main outcomes were performed by using the software package SSPS v20.
Results
1251 patients were included, 782 patients in the first period and 469 in the second one (main clinical features are shown in Table 1). E-alerts v2.0 was associated with an increase of appropriate LMWH prophylaxis during hospitalisation (65.2% vs 72.2%; p=0.015). However, this improvement did not result in a reduction of VTE during admission or follow-up (2.3% vs 2.3%; p=0.89). Interestingly, almost 80% of VTE events occurred despite LMWH use. No differences in the rate of major bleeding (2.8% vs 3.2%; p=0.83), and mortality (10.6% vs 14.3%; p=0.07) were observed, either. The main reason for not prescribing LMWH prophylaxis was bleeding risk, but in 17% of cases physicians did not consider that the patient really had a high VTE risk. No significant correlation was found between any of the clinical variables analyzed and the risk of VTE. Prophylaxis use was more frequent among patients with solid cancer (vs hematologic), advanced stage, active chemotherapy treatment and longer hospital stay.
Conclusion
The new e-alert system further increases the use of VTE prophylaxis in hospitalised cancer patients, although this was not associated with a reduction in the VTE incidence. A relevant number of VTE events occur despite prophylaxis with standard LMWH. Identificaton of risk factors for thromboprophylaxis failure is needed.
Session topic: 34. Thrombosis and vascular biology
Keyword(s): Venous thromboembolism, Thromboprophylaxis, Cancer


