
Contributions
Abstract: S112
Type: Oral Presentation
Presentation during EHA22: On Friday, June 23, 2017 from 12:00 - 12:15
Location: Hall C
Background
The detection of minimal residual disease (MRD) in patients with acute myeloid leukemia (AML) may improve future risk-adapted strategies of AML treatment. The presence of MRD after induction treatment has firmly been shown to predict for relapse and overall outcome, irrespective of type of post-remission treatment (PRT). Currently it is unknown whether and how the presence or absence of MRD should guide the application of allogeneic hematopoietic stem cell transplantation (alloHSCT) as PRT.
Aims
Methods
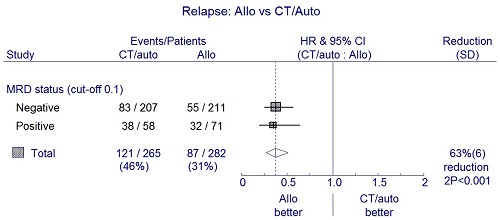
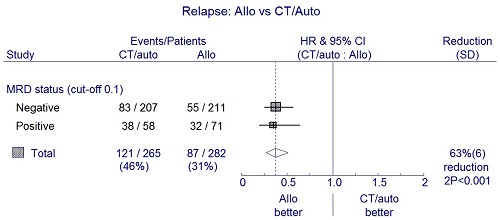
A total of 1,511 patients were treated in subsequent HOVON-SAKK AML trials of whom 547 patients obtained a CR1, received PRT and had available flow cytometric MRD prior to PRT. MRD positivity was defined by more than 0.1% cells with a leukemia associated phenotype within the white blood cell compartment. MRD status was not known by clinicians during AML treatment. PRT consisted of alloHSCT (n=282), or conventional PRT by a third cycle of chemotherapy (n=160) or autologous HSCT (n=105). Endpoints of the study included overall survival (OS), relapse-free survival (RFS), and cumulative incidences of relapse and non-relapse mortality (NRM) at 4 years. A time-dependent analysis was performed by applying multivariable Cox regression with time-dependent covariate alloHSCT with the cumulative incidence of relapse as primary endpoint.
Results
Conclusion
The graft-versus-leukemia effect of alloHSCT is equally present in MRD positive and MRD negative patients, which advocates a personalized application of alloHSCT taking the risk of relapse determined by AML risk group and MRD status as well as the counterbalancing risk of NRM into account.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Minimal residual disease (MRD), Graft-versus-leukemia, Allogeneic hematopoietic stem cell transplant, Acute Myeloid Leukemia
Abstract: S112
Type: Oral Presentation
Presentation during EHA22: On Friday, June 23, 2017 from 12:00 - 12:15
Location: Hall C
Background
The detection of minimal residual disease (MRD) in patients with acute myeloid leukemia (AML) may improve future risk-adapted strategies of AML treatment. The presence of MRD after induction treatment has firmly been shown to predict for relapse and overall outcome, irrespective of type of post-remission treatment (PRT). Currently it is unknown whether and how the presence or absence of MRD should guide the application of allogeneic hematopoietic stem cell transplantation (alloHSCT) as PRT.
Aims
Methods
A total of 1,511 patients were treated in subsequent HOVON-SAKK AML trials of whom 547 patients obtained a CR1, received PRT and had available flow cytometric MRD prior to PRT. MRD positivity was defined by more than 0.1% cells with a leukemia associated phenotype within the white blood cell compartment. MRD status was not known by clinicians during AML treatment. PRT consisted of alloHSCT (n=282), or conventional PRT by a third cycle of chemotherapy (n=160) or autologous HSCT (n=105). Endpoints of the study included overall survival (OS), relapse-free survival (RFS), and cumulative incidences of relapse and non-relapse mortality (NRM) at 4 years. A time-dependent analysis was performed by applying multivariable Cox regression with time-dependent covariate alloHSCT with the cumulative incidence of relapse as primary endpoint.
Results
Conclusion
The graft-versus-leukemia effect of alloHSCT is equally present in MRD positive and MRD negative patients, which advocates a personalized application of alloHSCT taking the risk of relapse determined by AML risk group and MRD status as well as the counterbalancing risk of NRM into account.
Session topic: 4. Acute myeloid leukemia - Clinical
Keyword(s): Minimal residual disease (MRD), Graft-versus-leukemia, Allogeneic hematopoietic stem cell transplant, Acute Myeloid Leukemia


