INCREASED RISK OF SECOND MALIGNANCIES IN PATIENTS WITH MYELOPROLIFERATIVE NEOPLASMS DIAGNOSED IN SWEDEN 1973-2009 ? A POPULATION-BASED COHORT STUDY OF 9,379 PATIENTS
(Abstract release date: 05/19/16)
EHA Library. Ravn Landtblom A. 06/10/16; 135144; S111

Dr. Anna Ravn Landtblom
Contributions
Contributions
Abstract
Abstract: S111
Type: Oral Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 11:45 - 12:00
Location: Auditorium 1
Background
The risk of developing acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) in patients with myeloproliferative neoplasms (MPNs) is well established. Less is known, however, about the risk of non-hematologic malignancies in patients with MPNs.
Aims
To assess the risk of developing a wide range of second malignancies in a large population-based study of MPN patients compared to matched controls.
Methods
All patients diagnosed with MPNs and reported to the Swedish Cancer Registry or the Inpatient Registry between 1973 and 2009 were included. Four controls matched by age, sex, and region of residence were randomly selected from the Register of Total Population. End of follow-up was December 31st 2010. Patients and controls were excluded if they had any malignancy prior to the MPN diagnosis or corresponding time for controls. We identified incident cases of cancer during follow-up by cross-linking to the Swedish Cancer Registry. Hazard ratios (HRs) with 95 % confidence intervals (CIs) were calculated using a Cox regression model. A landmark analysis was performed in order to reduce detection bias, where all patients with a new malignant diagnosis within one and two years respectively from the MPN diagnosis were excluded.
Results
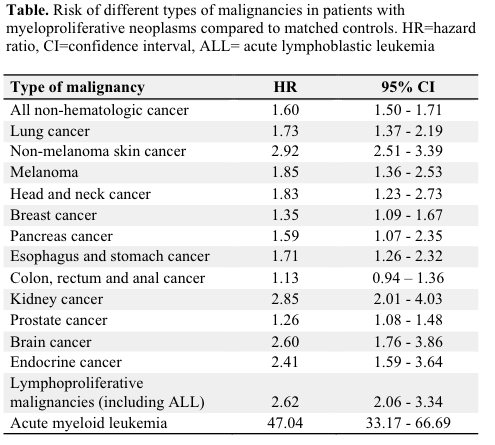
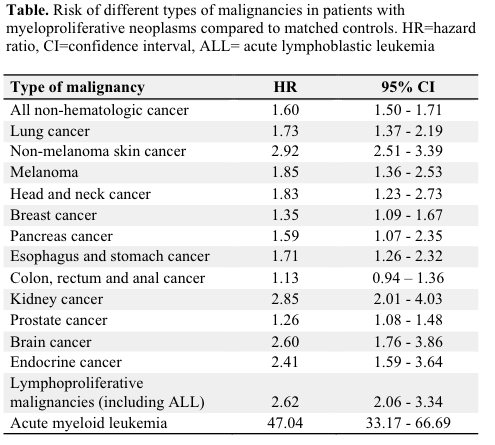
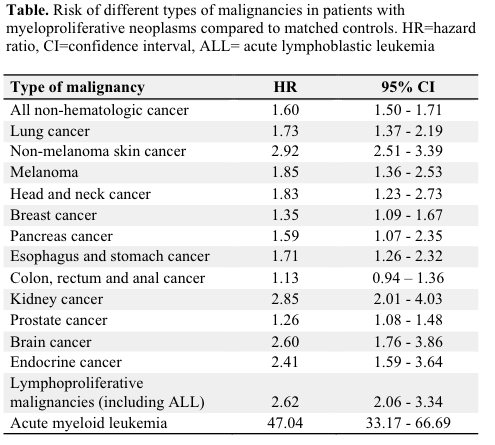
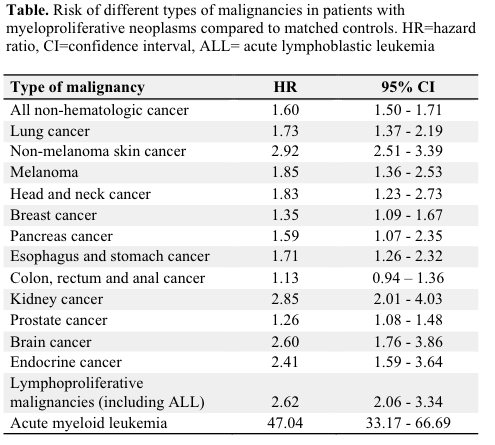
In total, 9,379 MPN patients and 35,682 controls were identified. The MPN cohort included 4,502 males (48%) and 4,877 females (52%), and the median age at MPN diagnosis was 67.5 years. We found an overall significantly increased risk of non-hematologic cancer with an HR of 1.60 (95 % CI 1.50-1.71). The relative risk of developing a second malignancy was similar across all MPN subtypes, men and women, and calendar periods of MPN diagnosis. The non-hematologic malignancies with the greatest observed risk increase included non-melanoma skin cancer (HR 2.92, 2.51-3.39), malignant melanoma (HR 1.85, 1.36-2.53), kidney cancer (HR 2.85, 2.01-4.03), brain cancer (HR 2.60, 1.76-3.86), and endocrine cancers including thyroid cancer HR 2.41, 1.59-3.64) (Table). MPN patients were also at a significantly increased risk of developing second malignancies of the lung, head and neck, pancreas, esophagus, and stomach compared to matched controls. The risk of developing a non-hematologic malignancy tended to increase with follow-up time after MPN diagnosis.The risk of developing a second hematologic malignancy was significantly increased, the HRs for lymphoproliferative malignancies (including acute lymphoblastic leukemia) were 2.62 (2.06-3.34) and for AML 47.04 (33.17-66.69). The relative risk of a second non-hematological and hematological malignancies in MPN patients remained similarly significantly elevated in the landmark analysis starting one and two years after the MPN diagnosis.
Conclusion
This population-based study is, to our knowledge, the largest to date to support an increased risk of non-hematologic and hematologic malignancies in MPN patients. The reason behind the increased risk are not fully understood, but several possible factors exist; a genetic propensity to develop malignancies, acquired somatic mutations, an altered immune function and mutagenic cytoreductive treatments. Clinicians should be aware of the increased cancer risk and direct adequate attention to new symptoms in MPN patients.
Session topic: Myeloproliferative neoplasms - Clinical 1
Keyword(s): Essential Thrombocytemia, Myelofibrosis, Polycythemia vera, Second malignancy
Type: Oral Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 11:45 - 12:00
Location: Auditorium 1
Background
The risk of developing acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) in patients with myeloproliferative neoplasms (MPNs) is well established. Less is known, however, about the risk of non-hematologic malignancies in patients with MPNs.
Aims
To assess the risk of developing a wide range of second malignancies in a large population-based study of MPN patients compared to matched controls.
Methods
All patients diagnosed with MPNs and reported to the Swedish Cancer Registry or the Inpatient Registry between 1973 and 2009 were included. Four controls matched by age, sex, and region of residence were randomly selected from the Register of Total Population. End of follow-up was December 31st 2010. Patients and controls were excluded if they had any malignancy prior to the MPN diagnosis or corresponding time for controls. We identified incident cases of cancer during follow-up by cross-linking to the Swedish Cancer Registry. Hazard ratios (HRs) with 95 % confidence intervals (CIs) were calculated using a Cox regression model. A landmark analysis was performed in order to reduce detection bias, where all patients with a new malignant diagnosis within one and two years respectively from the MPN diagnosis were excluded.
Results
In total, 9,379 MPN patients and 35,682 controls were identified. The MPN cohort included 4,502 males (48%) and 4,877 females (52%), and the median age at MPN diagnosis was 67.5 years. We found an overall significantly increased risk of non-hematologic cancer with an HR of 1.60 (95 % CI 1.50-1.71). The relative risk of developing a second malignancy was similar across all MPN subtypes, men and women, and calendar periods of MPN diagnosis. The non-hematologic malignancies with the greatest observed risk increase included non-melanoma skin cancer (HR 2.92, 2.51-3.39), malignant melanoma (HR 1.85, 1.36-2.53), kidney cancer (HR 2.85, 2.01-4.03), brain cancer (HR 2.60, 1.76-3.86), and endocrine cancers including thyroid cancer HR 2.41, 1.59-3.64) (Table). MPN patients were also at a significantly increased risk of developing second malignancies of the lung, head and neck, pancreas, esophagus, and stomach compared to matched controls. The risk of developing a non-hematologic malignancy tended to increase with follow-up time after MPN diagnosis.The risk of developing a second hematologic malignancy was significantly increased, the HRs for lymphoproliferative malignancies (including acute lymphoblastic leukemia) were 2.62 (2.06-3.34) and for AML 47.04 (33.17-66.69). The relative risk of a second non-hematological and hematological malignancies in MPN patients remained similarly significantly elevated in the landmark analysis starting one and two years after the MPN diagnosis.
Conclusion
This population-based study is, to our knowledge, the largest to date to support an increased risk of non-hematologic and hematologic malignancies in MPN patients. The reason behind the increased risk are not fully understood, but several possible factors exist; a genetic propensity to develop malignancies, acquired somatic mutations, an altered immune function and mutagenic cytoreductive treatments. Clinicians should be aware of the increased cancer risk and direct adequate attention to new symptoms in MPN patients.
Session topic: Myeloproliferative neoplasms - Clinical 1
Keyword(s): Essential Thrombocytemia, Myelofibrosis, Polycythemia vera, Second malignancy
Abstract: S111
Type: Oral Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 11:45 - 12:00
Location: Auditorium 1
Background
The risk of developing acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) in patients with myeloproliferative neoplasms (MPNs) is well established. Less is known, however, about the risk of non-hematologic malignancies in patients with MPNs.
Aims
To assess the risk of developing a wide range of second malignancies in a large population-based study of MPN patients compared to matched controls.
Methods
All patients diagnosed with MPNs and reported to the Swedish Cancer Registry or the Inpatient Registry between 1973 and 2009 were included. Four controls matched by age, sex, and region of residence were randomly selected from the Register of Total Population. End of follow-up was December 31st 2010. Patients and controls were excluded if they had any malignancy prior to the MPN diagnosis or corresponding time for controls. We identified incident cases of cancer during follow-up by cross-linking to the Swedish Cancer Registry. Hazard ratios (HRs) with 95 % confidence intervals (CIs) were calculated using a Cox regression model. A landmark analysis was performed in order to reduce detection bias, where all patients with a new malignant diagnosis within one and two years respectively from the MPN diagnosis were excluded.
Results
In total, 9,379 MPN patients and 35,682 controls were identified. The MPN cohort included 4,502 males (48%) and 4,877 females (52%), and the median age at MPN diagnosis was 67.5 years. We found an overall significantly increased risk of non-hematologic cancer with an HR of 1.60 (95 % CI 1.50-1.71). The relative risk of developing a second malignancy was similar across all MPN subtypes, men and women, and calendar periods of MPN diagnosis. The non-hematologic malignancies with the greatest observed risk increase included non-melanoma skin cancer (HR 2.92, 2.51-3.39), malignant melanoma (HR 1.85, 1.36-2.53), kidney cancer (HR 2.85, 2.01-4.03), brain cancer (HR 2.60, 1.76-3.86), and endocrine cancers including thyroid cancer HR 2.41, 1.59-3.64) (Table). MPN patients were also at a significantly increased risk of developing second malignancies of the lung, head and neck, pancreas, esophagus, and stomach compared to matched controls. The risk of developing a non-hematologic malignancy tended to increase with follow-up time after MPN diagnosis.The risk of developing a second hematologic malignancy was significantly increased, the HRs for lymphoproliferative malignancies (including acute lymphoblastic leukemia) were 2.62 (2.06-3.34) and for AML 47.04 (33.17-66.69). The relative risk of a second non-hematological and hematological malignancies in MPN patients remained similarly significantly elevated in the landmark analysis starting one and two years after the MPN diagnosis.
Conclusion
This population-based study is, to our knowledge, the largest to date to support an increased risk of non-hematologic and hematologic malignancies in MPN patients. The reason behind the increased risk are not fully understood, but several possible factors exist; a genetic propensity to develop malignancies, acquired somatic mutations, an altered immune function and mutagenic cytoreductive treatments. Clinicians should be aware of the increased cancer risk and direct adequate attention to new symptoms in MPN patients.
Session topic: Myeloproliferative neoplasms - Clinical 1
Keyword(s): Essential Thrombocytemia, Myelofibrosis, Polycythemia vera, Second malignancy
Type: Oral Presentation
Presentation during EHA21: On Friday, June 10, 2016 from 11:45 - 12:00
Location: Auditorium 1
Background
The risk of developing acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) in patients with myeloproliferative neoplasms (MPNs) is well established. Less is known, however, about the risk of non-hematologic malignancies in patients with MPNs.
Aims
To assess the risk of developing a wide range of second malignancies in a large population-based study of MPN patients compared to matched controls.
Methods
All patients diagnosed with MPNs and reported to the Swedish Cancer Registry or the Inpatient Registry between 1973 and 2009 were included. Four controls matched by age, sex, and region of residence were randomly selected from the Register of Total Population. End of follow-up was December 31st 2010. Patients and controls were excluded if they had any malignancy prior to the MPN diagnosis or corresponding time for controls. We identified incident cases of cancer during follow-up by cross-linking to the Swedish Cancer Registry. Hazard ratios (HRs) with 95 % confidence intervals (CIs) were calculated using a Cox regression model. A landmark analysis was performed in order to reduce detection bias, where all patients with a new malignant diagnosis within one and two years respectively from the MPN diagnosis were excluded.
Results
In total, 9,379 MPN patients and 35,682 controls were identified. The MPN cohort included 4,502 males (48%) and 4,877 females (52%), and the median age at MPN diagnosis was 67.5 years. We found an overall significantly increased risk of non-hematologic cancer with an HR of 1.60 (95 % CI 1.50-1.71). The relative risk of developing a second malignancy was similar across all MPN subtypes, men and women, and calendar periods of MPN diagnosis. The non-hematologic malignancies with the greatest observed risk increase included non-melanoma skin cancer (HR 2.92, 2.51-3.39), malignant melanoma (HR 1.85, 1.36-2.53), kidney cancer (HR 2.85, 2.01-4.03), brain cancer (HR 2.60, 1.76-3.86), and endocrine cancers including thyroid cancer HR 2.41, 1.59-3.64) (Table). MPN patients were also at a significantly increased risk of developing second malignancies of the lung, head and neck, pancreas, esophagus, and stomach compared to matched controls. The risk of developing a non-hematologic malignancy tended to increase with follow-up time after MPN diagnosis.The risk of developing a second hematologic malignancy was significantly increased, the HRs for lymphoproliferative malignancies (including acute lymphoblastic leukemia) were 2.62 (2.06-3.34) and for AML 47.04 (33.17-66.69). The relative risk of a second non-hematological and hematological malignancies in MPN patients remained similarly significantly elevated in the landmark analysis starting one and two years after the MPN diagnosis.
Conclusion
This population-based study is, to our knowledge, the largest to date to support an increased risk of non-hematologic and hematologic malignancies in MPN patients. The reason behind the increased risk are not fully understood, but several possible factors exist; a genetic propensity to develop malignancies, acquired somatic mutations, an altered immune function and mutagenic cytoreductive treatments. Clinicians should be aware of the increased cancer risk and direct adequate attention to new symptoms in MPN patients.
Session topic: Myeloproliferative neoplasms - Clinical 1
Keyword(s): Essential Thrombocytemia, Myelofibrosis, Polycythemia vera, Second malignancy
{{ help_message }}
{{filter}}


