ANTIPHOSPHOLIPID ANTIBODIES, PREGNANCY AND SPONTANEOUS MISCARRIAGES. EXPERIENCE FROM A RECENTLY OPENED CENTER.
(Abstract release date: 05/19/16)
EHA Library. muñoz C. 06/09/16; 135109; PB2209

Dr. Carolina muñoz
Contributions
Contributions
Abstract
Abstract: PB2209
Type: Publication Only
Background
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by the appearance of arterial or venous thrombotic events and / or obstetric complications in the presence of antiphospholipid antibodies (aPL). These include: lupus anticoagulant (LA), anticardiolipin antibodies (aCL), and anti-beta2 glycoprotein I antibodies (aβ2GPI). APLs are found in up to 40% of women who suffer recurrent miscarriages and/or fetal deaths. LA has been associated with preeclampsia, intrauterine growth retardation (IUGR) and fetal loss. ACA are linked to preeclampsia and late fetal loss. The aβ2GPI to preeclampsia, IUGR and late fetal loss. The presence of any of them in pregnancy is a predictor of adverse outcome and should be considered a high risk factor for venous thromboembolism (VTE). The management of these patients could be controversial, especially in cases with moderate-high titles of LA and/or aCL with neither thrombotic nor obstetric signs, although this approach has not been tested in prospective clinical trials. The combined therapy of acetylsalicylic acid (ASA) and low molecular weight heparin (LMWH) has shown efficacy and birth rates close to 80%, with less toxicity than other schemes including corticosteroids and/or immunoglobulins
Aims
determine the prevalence and clinical significance of the aPL in women with recurrent miscarriages and obstetric complications
Methods
Retrospective analysis of patients with a previous history of recurrent miscarriages or fetal deaths, between 2009 and 2015, referred to the hematology consultation in which the presence of aPL was confirmed in two separate determinations at least 12 weeks apart
Results
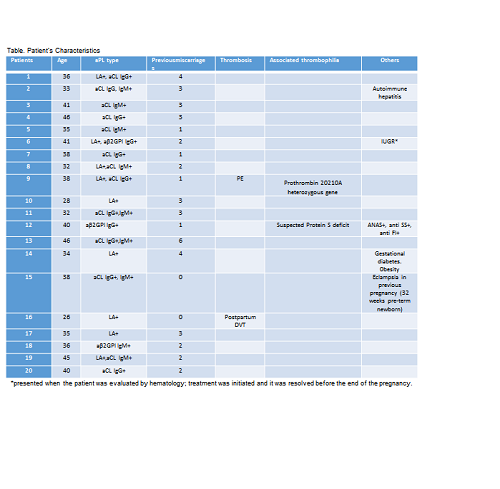
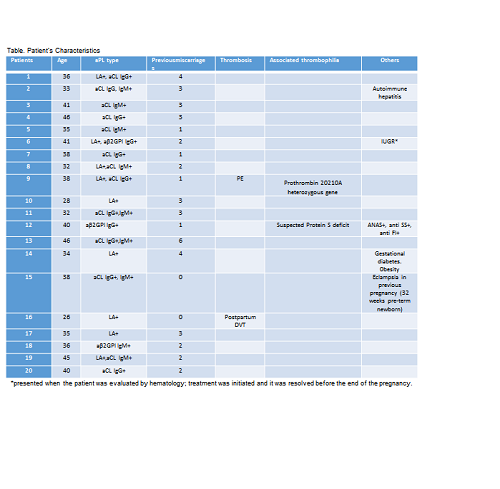
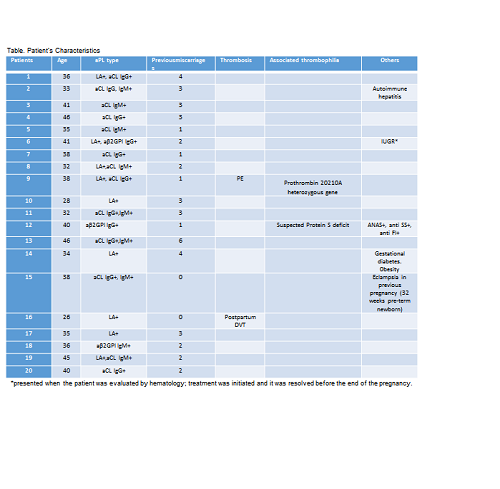
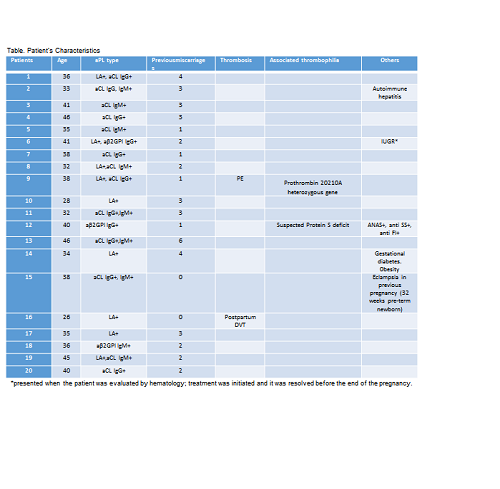
The presence of aPL was confirmed in 20 patients and 13 were diagnosed according to the Sydney classification criteria for APS. The accompanying clinical manifestations in those patients with positive aPL were: recurrent miscarriages in 18/20 (90%), median of 3 abortions <12 weeks; VTE disease 2/20 (10%); 1 patient with a history of fetal loss at 24 weeks; 1case of eclampsia in previous pregnancy and 1 case of IUGR (See table).The antibody most frequently involved was aCL, present in 13/20 (65%). The LA was observed in 9/20 (45%), including this group, the only 2 cases with VTE in the series and the only case with IUGR. 25% (5/20) of the patients had more than one positive aPL, one of these patients had having a previous history of pulmonary embolism (PE) before the diagnosis of APS. After the diagnosis of APS 18/20 cases (90%) had new pregnancies including 15 full-term newborns and 3 ongoing pregnancies. All these patients were treated with ASA and LMWH at prophylactic doses, with monitoring levels of anti-Xa. Once treatment was established the only complication was one pregnancy loss at weeks eight of gestation in an obese patient who did not reach levels of anti-Xa at prophylactic range, but later had a successful pregnancy by increasing the dose of LMWH. There were no fetal deaths or new cases of VTE or hemorrhagic complications.
Conclusion
Combination therapy with ASA and LMWH is safe and effective in the secondary prevention of obstetric complications in patients with APS. As in other series, our study confirms that more than one positive aPL determination and LA positivity are associated with an increase of the number and severity of complications in patients with APS. Further studies to improve the current evidence for the management of these patients are needed
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Autoimmune disease, Pregnancy, Venous thromboembolism
Type: Publication Only
Background
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by the appearance of arterial or venous thrombotic events and / or obstetric complications in the presence of antiphospholipid antibodies (aPL). These include: lupus anticoagulant (LA), anticardiolipin antibodies (aCL), and anti-beta2 glycoprotein I antibodies (aβ2GPI). APLs are found in up to 40% of women who suffer recurrent miscarriages and/or fetal deaths. LA has been associated with preeclampsia, intrauterine growth retardation (IUGR) and fetal loss. ACA are linked to preeclampsia and late fetal loss. The aβ2GPI to preeclampsia, IUGR and late fetal loss. The presence of any of them in pregnancy is a predictor of adverse outcome and should be considered a high risk factor for venous thromboembolism (VTE). The management of these patients could be controversial, especially in cases with moderate-high titles of LA and/or aCL with neither thrombotic nor obstetric signs, although this approach has not been tested in prospective clinical trials. The combined therapy of acetylsalicylic acid (ASA) and low molecular weight heparin (LMWH) has shown efficacy and birth rates close to 80%, with less toxicity than other schemes including corticosteroids and/or immunoglobulins
Aims
determine the prevalence and clinical significance of the aPL in women with recurrent miscarriages and obstetric complications
Methods
Retrospective analysis of patients with a previous history of recurrent miscarriages or fetal deaths, between 2009 and 2015, referred to the hematology consultation in which the presence of aPL was confirmed in two separate determinations at least 12 weeks apart
Results
The presence of aPL was confirmed in 20 patients and 13 were diagnosed according to the Sydney classification criteria for APS. The accompanying clinical manifestations in those patients with positive aPL were: recurrent miscarriages in 18/20 (90%), median of 3 abortions <12 weeks; VTE disease 2/20 (10%); 1 patient with a history of fetal loss at 24 weeks; 1case of eclampsia in previous pregnancy and 1 case of IUGR (See table).The antibody most frequently involved was aCL, present in 13/20 (65%). The LA was observed in 9/20 (45%), including this group, the only 2 cases with VTE in the series and the only case with IUGR. 25% (5/20) of the patients had more than one positive aPL, one of these patients had having a previous history of pulmonary embolism (PE) before the diagnosis of APS. After the diagnosis of APS 18/20 cases (90%) had new pregnancies including 15 full-term newborns and 3 ongoing pregnancies. All these patients were treated with ASA and LMWH at prophylactic doses, with monitoring levels of anti-Xa. Once treatment was established the only complication was one pregnancy loss at weeks eight of gestation in an obese patient who did not reach levels of anti-Xa at prophylactic range, but later had a successful pregnancy by increasing the dose of LMWH. There were no fetal deaths or new cases of VTE or hemorrhagic complications.
Conclusion
Combination therapy with ASA and LMWH is safe and effective in the secondary prevention of obstetric complications in patients with APS. As in other series, our study confirms that more than one positive aPL determination and LA positivity are associated with an increase of the number and severity of complications in patients with APS. Further studies to improve the current evidence for the management of these patients are needed
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Autoimmune disease, Pregnancy, Venous thromboembolism
Abstract: PB2209
Type: Publication Only
Background
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by the appearance of arterial or venous thrombotic events and / or obstetric complications in the presence of antiphospholipid antibodies (aPL). These include: lupus anticoagulant (LA), anticardiolipin antibodies (aCL), and anti-beta2 glycoprotein I antibodies (aβ2GPI). APLs are found in up to 40% of women who suffer recurrent miscarriages and/or fetal deaths. LA has been associated with preeclampsia, intrauterine growth retardation (IUGR) and fetal loss. ACA are linked to preeclampsia and late fetal loss. The aβ2GPI to preeclampsia, IUGR and late fetal loss. The presence of any of them in pregnancy is a predictor of adverse outcome and should be considered a high risk factor for venous thromboembolism (VTE). The management of these patients could be controversial, especially in cases with moderate-high titles of LA and/or aCL with neither thrombotic nor obstetric signs, although this approach has not been tested in prospective clinical trials. The combined therapy of acetylsalicylic acid (ASA) and low molecular weight heparin (LMWH) has shown efficacy and birth rates close to 80%, with less toxicity than other schemes including corticosteroids and/or immunoglobulins
Aims
determine the prevalence and clinical significance of the aPL in women with recurrent miscarriages and obstetric complications
Methods
Retrospective analysis of patients with a previous history of recurrent miscarriages or fetal deaths, between 2009 and 2015, referred to the hematology consultation in which the presence of aPL was confirmed in two separate determinations at least 12 weeks apart
Results
The presence of aPL was confirmed in 20 patients and 13 were diagnosed according to the Sydney classification criteria for APS. The accompanying clinical manifestations in those patients with positive aPL were: recurrent miscarriages in 18/20 (90%), median of 3 abortions <12 weeks; VTE disease 2/20 (10%); 1 patient with a history of fetal loss at 24 weeks; 1case of eclampsia in previous pregnancy and 1 case of IUGR (See table).The antibody most frequently involved was aCL, present in 13/20 (65%). The LA was observed in 9/20 (45%), including this group, the only 2 cases with VTE in the series and the only case with IUGR. 25% (5/20) of the patients had more than one positive aPL, one of these patients had having a previous history of pulmonary embolism (PE) before the diagnosis of APS. After the diagnosis of APS 18/20 cases (90%) had new pregnancies including 15 full-term newborns and 3 ongoing pregnancies. All these patients were treated with ASA and LMWH at prophylactic doses, with monitoring levels of anti-Xa. Once treatment was established the only complication was one pregnancy loss at weeks eight of gestation in an obese patient who did not reach levels of anti-Xa at prophylactic range, but later had a successful pregnancy by increasing the dose of LMWH. There were no fetal deaths or new cases of VTE or hemorrhagic complications.
Conclusion
Combination therapy with ASA and LMWH is safe and effective in the secondary prevention of obstetric complications in patients with APS. As in other series, our study confirms that more than one positive aPL determination and LA positivity are associated with an increase of the number and severity of complications in patients with APS. Further studies to improve the current evidence for the management of these patients are needed
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Autoimmune disease, Pregnancy, Venous thromboembolism
Type: Publication Only
Background
Antiphospholipid syndrome (APS) is an autoimmune disorder characterized by the appearance of arterial or venous thrombotic events and / or obstetric complications in the presence of antiphospholipid antibodies (aPL). These include: lupus anticoagulant (LA), anticardiolipin antibodies (aCL), and anti-beta2 glycoprotein I antibodies (aβ2GPI). APLs are found in up to 40% of women who suffer recurrent miscarriages and/or fetal deaths. LA has been associated with preeclampsia, intrauterine growth retardation (IUGR) and fetal loss. ACA are linked to preeclampsia and late fetal loss. The aβ2GPI to preeclampsia, IUGR and late fetal loss. The presence of any of them in pregnancy is a predictor of adverse outcome and should be considered a high risk factor for venous thromboembolism (VTE). The management of these patients could be controversial, especially in cases with moderate-high titles of LA and/or aCL with neither thrombotic nor obstetric signs, although this approach has not been tested in prospective clinical trials. The combined therapy of acetylsalicylic acid (ASA) and low molecular weight heparin (LMWH) has shown efficacy and birth rates close to 80%, with less toxicity than other schemes including corticosteroids and/or immunoglobulins
Aims
determine the prevalence and clinical significance of the aPL in women with recurrent miscarriages and obstetric complications
Methods
Retrospective analysis of patients with a previous history of recurrent miscarriages or fetal deaths, between 2009 and 2015, referred to the hematology consultation in which the presence of aPL was confirmed in two separate determinations at least 12 weeks apart
Results
The presence of aPL was confirmed in 20 patients and 13 were diagnosed according to the Sydney classification criteria for APS. The accompanying clinical manifestations in those patients with positive aPL were: recurrent miscarriages in 18/20 (90%), median of 3 abortions <12 weeks; VTE disease 2/20 (10%); 1 patient with a history of fetal loss at 24 weeks; 1case of eclampsia in previous pregnancy and 1 case of IUGR (See table).The antibody most frequently involved was aCL, present in 13/20 (65%). The LA was observed in 9/20 (45%), including this group, the only 2 cases with VTE in the series and the only case with IUGR. 25% (5/20) of the patients had more than one positive aPL, one of these patients had having a previous history of pulmonary embolism (PE) before the diagnosis of APS. After the diagnosis of APS 18/20 cases (90%) had new pregnancies including 15 full-term newborns and 3 ongoing pregnancies. All these patients were treated with ASA and LMWH at prophylactic doses, with monitoring levels of anti-Xa. Once treatment was established the only complication was one pregnancy loss at weeks eight of gestation in an obese patient who did not reach levels of anti-Xa at prophylactic range, but later had a successful pregnancy by increasing the dose of LMWH. There were no fetal deaths or new cases of VTE or hemorrhagic complications.
Conclusion
Combination therapy with ASA and LMWH is safe and effective in the secondary prevention of obstetric complications in patients with APS. As in other series, our study confirms that more than one positive aPL determination and LA positivity are associated with an increase of the number and severity of complications in patients with APS. Further studies to improve the current evidence for the management of these patients are needed
Session topic: E-poster
Keyword(s): Antiphospholipid antibody, Autoimmune disease, Pregnancy, Venous thromboembolism
{{ help_message }}
{{filter}}


