MRI PROSPECTIVE SURVEY ON CARDIAC IRON AND FUNCTION AND ON HEPATIC IRON IN NON TRANSFUSION-DEPENDENT THALASSEMIA INTERMEDIA PATIENTS TREATED WITH DESFERRIOXAMINE OR NON CHELATED.
(Abstract release date: 05/19/16)
EHA Library. Meloni A. 06/09/16; 135046; PB2146

Dr. Antonella Meloni
Contributions
Contributions
Abstract
Abstract: PB2146
Type: Publication Only
Background
Few studies have evaluated the efficacy of iron chelation therapy in thalassemia intermedia (TI) patients.
Aims
Our study aimed to prospectively assess by quantitative Magnetic Resonance imaging (MRI) the efficacy of Desferrioxamine (DFO) and its advantages with respect to the absence of chelation therapy in non transfusion-dependent (NTD) TI patients.
Methods
Among the 185 TI patients enrolled in the MIOT (Myocardial Iron Overload in Thalassemia) network and with a MRI follow-up (FU) study at 18±3 months, we selected 65 NTD patients. Cardiac iron overload was assessed by the multislice multiecho T2* technique. LV function parameters were quantified by cine SSFP sequences. Liver T2* values were converted into liver iron concentration (LIC) values.
Results
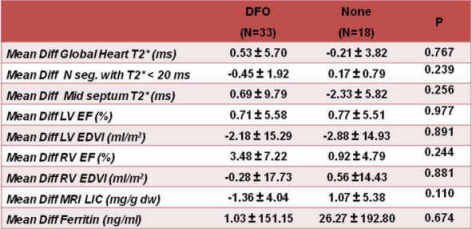
We considered 18 patients who have not received any chelation therapy (50% males; mean age: 37.83±14.29 years) and 33 patients who had received DFO alone between the two MRI scans (51.5% males; mean age: 38.85±7.83 years). The two groups were comparable for age, sex and baseline MRI data.No patient treated with DFO had cardiac iron. At baseline only one non-chelated patient showed a pathological global heart T2* value (<20 ms) and he recovered at the FU. The percentage of patients who maintained a normal global heart T2* value was 100% in both groups. A significant increase in the right ventricular ejection fraction was detected in DFO patients (-3.48 ± 7.22%; P=0.024). The changes in cardiac T2* values and in the global systolic biventricular function were not significantly different between the two groups (Table 1).In patients with hepatic iron at baseline (MRI LIC ≥3 mg/g/dw), the reduction in the MRI LIC values was significant only in the DFO group (-2.20±4.84 mg/g/dw; P=0.050). The decrease in MRI LIC values was comparable between the groups (P=0.155).
Conclusion
In this small population of sporadically or non transfused TI patients, DFO therapy showed no advantage in terms of cardiac iron but its administration allowed and improvement in right ventricular function and hepatic iron overload.
Session topic: E-poster
Keyword(s): Chelation, Magnetic resonance imaging, Thalassemia
Type: Publication Only
Background
Few studies have evaluated the efficacy of iron chelation therapy in thalassemia intermedia (TI) patients.
Aims
Our study aimed to prospectively assess by quantitative Magnetic Resonance imaging (MRI) the efficacy of Desferrioxamine (DFO) and its advantages with respect to the absence of chelation therapy in non transfusion-dependent (NTD) TI patients.
Methods
Among the 185 TI patients enrolled in the MIOT (Myocardial Iron Overload in Thalassemia) network and with a MRI follow-up (FU) study at 18±3 months, we selected 65 NTD patients. Cardiac iron overload was assessed by the multislice multiecho T2* technique. LV function parameters were quantified by cine SSFP sequences. Liver T2* values were converted into liver iron concentration (LIC) values.
Results
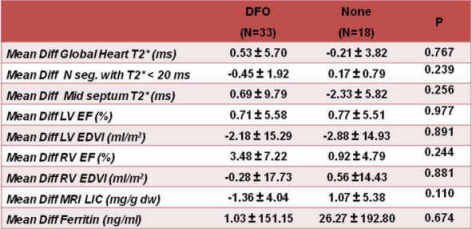
We considered 18 patients who have not received any chelation therapy (50% males; mean age: 37.83±14.29 years) and 33 patients who had received DFO alone between the two MRI scans (51.5% males; mean age: 38.85±7.83 years). The two groups were comparable for age, sex and baseline MRI data.No patient treated with DFO had cardiac iron. At baseline only one non-chelated patient showed a pathological global heart T2* value (<20 ms) and he recovered at the FU. The percentage of patients who maintained a normal global heart T2* value was 100% in both groups. A significant increase in the right ventricular ejection fraction was detected in DFO patients (-3.48 ± 7.22%; P=0.024). The changes in cardiac T2* values and in the global systolic biventricular function were not significantly different between the two groups (Table 1).In patients with hepatic iron at baseline (MRI LIC ≥3 mg/g/dw), the reduction in the MRI LIC values was significant only in the DFO group (-2.20±4.84 mg/g/dw; P=0.050). The decrease in MRI LIC values was comparable between the groups (P=0.155).
Conclusion
In this small population of sporadically or non transfused TI patients, DFO therapy showed no advantage in terms of cardiac iron but its administration allowed and improvement in right ventricular function and hepatic iron overload.
Session topic: E-poster
Keyword(s): Chelation, Magnetic resonance imaging, Thalassemia
Abstract: PB2146
Type: Publication Only
Background
Few studies have evaluated the efficacy of iron chelation therapy in thalassemia intermedia (TI) patients.
Aims
Our study aimed to prospectively assess by quantitative Magnetic Resonance imaging (MRI) the efficacy of Desferrioxamine (DFO) and its advantages with respect to the absence of chelation therapy in non transfusion-dependent (NTD) TI patients.
Methods
Among the 185 TI patients enrolled in the MIOT (Myocardial Iron Overload in Thalassemia) network and with a MRI follow-up (FU) study at 18±3 months, we selected 65 NTD patients. Cardiac iron overload was assessed by the multislice multiecho T2* technique. LV function parameters were quantified by cine SSFP sequences. Liver T2* values were converted into liver iron concentration (LIC) values.
Results
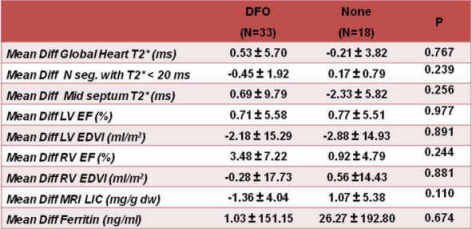
We considered 18 patients who have not received any chelation therapy (50% males; mean age: 37.83±14.29 years) and 33 patients who had received DFO alone between the two MRI scans (51.5% males; mean age: 38.85±7.83 years). The two groups were comparable for age, sex and baseline MRI data.No patient treated with DFO had cardiac iron. At baseline only one non-chelated patient showed a pathological global heart T2* value (<20 ms) and he recovered at the FU. The percentage of patients who maintained a normal global heart T2* value was 100% in both groups. A significant increase in the right ventricular ejection fraction was detected in DFO patients (-3.48 ± 7.22%; P=0.024). The changes in cardiac T2* values and in the global systolic biventricular function were not significantly different between the two groups (Table 1).In patients with hepatic iron at baseline (MRI LIC ≥3 mg/g/dw), the reduction in the MRI LIC values was significant only in the DFO group (-2.20±4.84 mg/g/dw; P=0.050). The decrease in MRI LIC values was comparable between the groups (P=0.155).
Conclusion
In this small population of sporadically or non transfused TI patients, DFO therapy showed no advantage in terms of cardiac iron but its administration allowed and improvement in right ventricular function and hepatic iron overload.
Session topic: E-poster
Keyword(s): Chelation, Magnetic resonance imaging, Thalassemia
Type: Publication Only
Background
Few studies have evaluated the efficacy of iron chelation therapy in thalassemia intermedia (TI) patients.
Aims
Our study aimed to prospectively assess by quantitative Magnetic Resonance imaging (MRI) the efficacy of Desferrioxamine (DFO) and its advantages with respect to the absence of chelation therapy in non transfusion-dependent (NTD) TI patients.
Methods
Among the 185 TI patients enrolled in the MIOT (Myocardial Iron Overload in Thalassemia) network and with a MRI follow-up (FU) study at 18±3 months, we selected 65 NTD patients. Cardiac iron overload was assessed by the multislice multiecho T2* technique. LV function parameters were quantified by cine SSFP sequences. Liver T2* values were converted into liver iron concentration (LIC) values.
Results
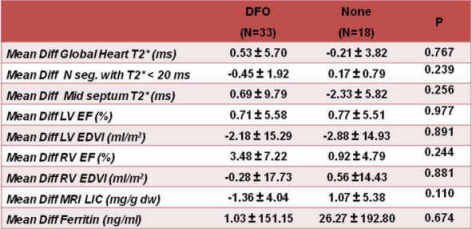
We considered 18 patients who have not received any chelation therapy (50% males; mean age: 37.83±14.29 years) and 33 patients who had received DFO alone between the two MRI scans (51.5% males; mean age: 38.85±7.83 years). The two groups were comparable for age, sex and baseline MRI data.No patient treated with DFO had cardiac iron. At baseline only one non-chelated patient showed a pathological global heart T2* value (<20 ms) and he recovered at the FU. The percentage of patients who maintained a normal global heart T2* value was 100% in both groups. A significant increase in the right ventricular ejection fraction was detected in DFO patients (-3.48 ± 7.22%; P=0.024). The changes in cardiac T2* values and in the global systolic biventricular function were not significantly different between the two groups (Table 1).In patients with hepatic iron at baseline (MRI LIC ≥3 mg/g/dw), the reduction in the MRI LIC values was significant only in the DFO group (-2.20±4.84 mg/g/dw; P=0.050). The decrease in MRI LIC values was comparable between the groups (P=0.155).
Conclusion
In this small population of sporadically or non transfused TI patients, DFO therapy showed no advantage in terms of cardiac iron but its administration allowed and improvement in right ventricular function and hepatic iron overload.
Session topic: E-poster
Keyword(s): Chelation, Magnetic resonance imaging, Thalassemia
{{ help_message }}
{{filter}}


