IMPACT OF THE NAGASAKI ATOMIC BOMB ON THE INCIDENCE RATE AND OUTCOME OF FOLLICULAR LYMPHOMA
(Abstract release date: 05/19/16)
EHA Library. Jo T. 06/09/16; 134944; PB2044

Dr. Tatsuro Jo
Contributions
Contributions
Abstract
Abstract: PB2044
Type: Publication Only
Background
In Nagasaki and Hiroshima, approximately 75,000 and 120,000 citizens, respectively, died within 3 months of the 1945 atomic bomb explosions. Furthermore, 80,000 and 140,000 citizens, respectively, survived exposure. During the following 70 years, high-dose radiation exposure has induced various cancers, including leukemia; thyroid, lung, gastric, and colon cancers; and myelodysplastic syndromes (MDS). Additionally, approximately 10% of cancer-carrying patients of Nagasaki atomic bomb survivors have multiple primary cancers in various tissues. This high-dose radiation exposure not only increased the risk of developing various types of cancer, but also worsened the overall survival (OS) rate. We recently reported significantly shorter OS among Nagasaki atomic bomb survivors with MDS versus patients without such radiation exposure (Jo et al., Anticancer Research 2015).
Aims
We investigated whether high-dose radiation exposure would similarly affect the incidence rates and outcomes of follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL).
Methods
The youngest atomic bomb survivors are aged approximately 70 years, presenting a challenge to perform prospective cohort studies. Therefore, we conducted a retrospective cohort study of the incidence rates and outcomes of FL and DLBCL in cases diagnosed at our hospital between January 2004 and December 2013. The primary objectives were to compare the incidence rates of FL and DLBCL in atomic bomb survivors (A-Bomb) and non-A-Bomb patients, and determine the OS rates.
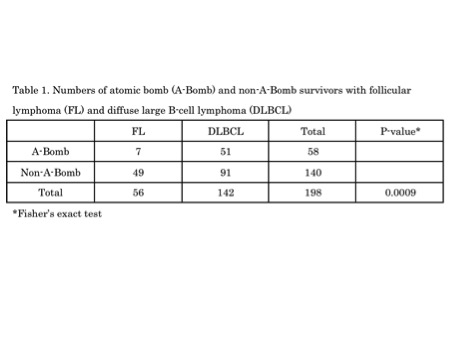
Results
Table 1 lists the number of patients. Seven and 51 A-Bomb patients and 49 and 91 non-A-Bomb patients had FL and DLBCL, respectively. The incidence rate of FL versus DLBCL was significantly less among A-Bomb patients than among non-A-Bomb patients (P = 0.0009). There was no significant difference in OS between A-Bomb and non-A-Bomb patients with DLBCL (P = 0.3065, hazard ration [HR]: 1.311, 95% confidence interval [CI]: 0.7813–2.198). In contrast to DLBCL, the OS rate was significantly lower in A-Bomb patients with FL than in non-A-Bomb patients (P = 0.0092, HR: 5.425, 95% CI: 2.151–220.1). In both FL and DLBCL patients, there were no significant differences of background factors except for the median age between A-Bomb and non-A-Bomb patients. The respective median ages of A-Bomb and non-A-Bomb patients with DLBCL differed significantly at 75 (range, 62–91) and 73 (range, 17–93) years (P = 0.0038). The respective median ages of A-Bomb and non-A-Bomb patients with FL also differed significantly at 80 (range, 63–90) and 60 (range, 28–80) years (P < 0.0001). The age difference had no impact on the OS rate of DLBCL. Therefore, the shorter OS of A-Bomb patients with FL cannot be accounted only for the age difference between A-Bomb and non-A-Bomb patients. Some other unknown factors caused by high-dose radiation exposure of the Nagasaki Atomic Bomb could be linked to the OS difference.
Conclusion
Compared with non-A-Bomb patients, A-Bomb patients had a significantly lower FL incidence rate and significantly shorter OS. We previously reported significantly reduced OS among MDS patients exposed to the Nagasaki atomic bomb. These data suggest an influence of atomic bomb exposure and warrant further study for etiological clarification.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Follicular lymphoma, Radiation
Type: Publication Only
Background
In Nagasaki and Hiroshima, approximately 75,000 and 120,000 citizens, respectively, died within 3 months of the 1945 atomic bomb explosions. Furthermore, 80,000 and 140,000 citizens, respectively, survived exposure. During the following 70 years, high-dose radiation exposure has induced various cancers, including leukemia; thyroid, lung, gastric, and colon cancers; and myelodysplastic syndromes (MDS). Additionally, approximately 10% of cancer-carrying patients of Nagasaki atomic bomb survivors have multiple primary cancers in various tissues. This high-dose radiation exposure not only increased the risk of developing various types of cancer, but also worsened the overall survival (OS) rate. We recently reported significantly shorter OS among Nagasaki atomic bomb survivors with MDS versus patients without such radiation exposure (Jo et al., Anticancer Research 2015).
Aims
We investigated whether high-dose radiation exposure would similarly affect the incidence rates and outcomes of follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL).
Methods
The youngest atomic bomb survivors are aged approximately 70 years, presenting a challenge to perform prospective cohort studies. Therefore, we conducted a retrospective cohort study of the incidence rates and outcomes of FL and DLBCL in cases diagnosed at our hospital between January 2004 and December 2013. The primary objectives were to compare the incidence rates of FL and DLBCL in atomic bomb survivors (A-Bomb) and non-A-Bomb patients, and determine the OS rates.
Results
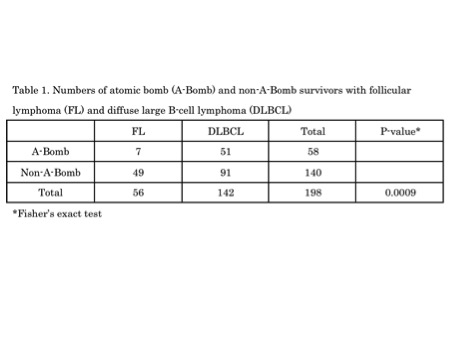
Table 1 lists the number of patients. Seven and 51 A-Bomb patients and 49 and 91 non-A-Bomb patients had FL and DLBCL, respectively. The incidence rate of FL versus DLBCL was significantly less among A-Bomb patients than among non-A-Bomb patients (P = 0.0009). There was no significant difference in OS between A-Bomb and non-A-Bomb patients with DLBCL (P = 0.3065, hazard ration [HR]: 1.311, 95% confidence interval [CI]: 0.7813–2.198). In contrast to DLBCL, the OS rate was significantly lower in A-Bomb patients with FL than in non-A-Bomb patients (P = 0.0092, HR: 5.425, 95% CI: 2.151–220.1). In both FL and DLBCL patients, there were no significant differences of background factors except for the median age between A-Bomb and non-A-Bomb patients. The respective median ages of A-Bomb and non-A-Bomb patients with DLBCL differed significantly at 75 (range, 62–91) and 73 (range, 17–93) years (P = 0.0038). The respective median ages of A-Bomb and non-A-Bomb patients with FL also differed significantly at 80 (range, 63–90) and 60 (range, 28–80) years (P < 0.0001). The age difference had no impact on the OS rate of DLBCL. Therefore, the shorter OS of A-Bomb patients with FL cannot be accounted only for the age difference between A-Bomb and non-A-Bomb patients. Some other unknown factors caused by high-dose radiation exposure of the Nagasaki Atomic Bomb could be linked to the OS difference.
Conclusion
Compared with non-A-Bomb patients, A-Bomb patients had a significantly lower FL incidence rate and significantly shorter OS. We previously reported significantly reduced OS among MDS patients exposed to the Nagasaki atomic bomb. These data suggest an influence of atomic bomb exposure and warrant further study for etiological clarification.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Follicular lymphoma, Radiation
Abstract: PB2044
Type: Publication Only
Background
In Nagasaki and Hiroshima, approximately 75,000 and 120,000 citizens, respectively, died within 3 months of the 1945 atomic bomb explosions. Furthermore, 80,000 and 140,000 citizens, respectively, survived exposure. During the following 70 years, high-dose radiation exposure has induced various cancers, including leukemia; thyroid, lung, gastric, and colon cancers; and myelodysplastic syndromes (MDS). Additionally, approximately 10% of cancer-carrying patients of Nagasaki atomic bomb survivors have multiple primary cancers in various tissues. This high-dose radiation exposure not only increased the risk of developing various types of cancer, but also worsened the overall survival (OS) rate. We recently reported significantly shorter OS among Nagasaki atomic bomb survivors with MDS versus patients without such radiation exposure (Jo et al., Anticancer Research 2015).
Aims
We investigated whether high-dose radiation exposure would similarly affect the incidence rates and outcomes of follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL).
Methods
The youngest atomic bomb survivors are aged approximately 70 years, presenting a challenge to perform prospective cohort studies. Therefore, we conducted a retrospective cohort study of the incidence rates and outcomes of FL and DLBCL in cases diagnosed at our hospital between January 2004 and December 2013. The primary objectives were to compare the incidence rates of FL and DLBCL in atomic bomb survivors (A-Bomb) and non-A-Bomb patients, and determine the OS rates.
Results
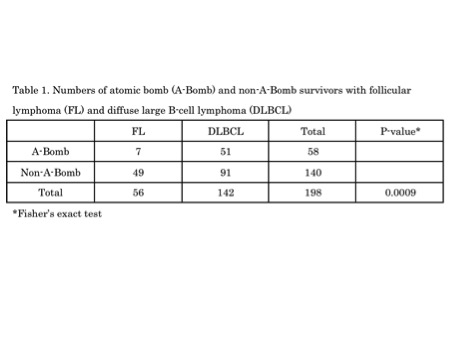
Table 1 lists the number of patients. Seven and 51 A-Bomb patients and 49 and 91 non-A-Bomb patients had FL and DLBCL, respectively. The incidence rate of FL versus DLBCL was significantly less among A-Bomb patients than among non-A-Bomb patients (P = 0.0009). There was no significant difference in OS between A-Bomb and non-A-Bomb patients with DLBCL (P = 0.3065, hazard ration [HR]: 1.311, 95% confidence interval [CI]: 0.7813–2.198). In contrast to DLBCL, the OS rate was significantly lower in A-Bomb patients with FL than in non-A-Bomb patients (P = 0.0092, HR: 5.425, 95% CI: 2.151–220.1). In both FL and DLBCL patients, there were no significant differences of background factors except for the median age between A-Bomb and non-A-Bomb patients. The respective median ages of A-Bomb and non-A-Bomb patients with DLBCL differed significantly at 75 (range, 62–91) and 73 (range, 17–93) years (P = 0.0038). The respective median ages of A-Bomb and non-A-Bomb patients with FL also differed significantly at 80 (range, 63–90) and 60 (range, 28–80) years (P < 0.0001). The age difference had no impact on the OS rate of DLBCL. Therefore, the shorter OS of A-Bomb patients with FL cannot be accounted only for the age difference between A-Bomb and non-A-Bomb patients. Some other unknown factors caused by high-dose radiation exposure of the Nagasaki Atomic Bomb could be linked to the OS difference.
Conclusion
Compared with non-A-Bomb patients, A-Bomb patients had a significantly lower FL incidence rate and significantly shorter OS. We previously reported significantly reduced OS among MDS patients exposed to the Nagasaki atomic bomb. These data suggest an influence of atomic bomb exposure and warrant further study for etiological clarification.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Follicular lymphoma, Radiation
Type: Publication Only
Background
In Nagasaki and Hiroshima, approximately 75,000 and 120,000 citizens, respectively, died within 3 months of the 1945 atomic bomb explosions. Furthermore, 80,000 and 140,000 citizens, respectively, survived exposure. During the following 70 years, high-dose radiation exposure has induced various cancers, including leukemia; thyroid, lung, gastric, and colon cancers; and myelodysplastic syndromes (MDS). Additionally, approximately 10% of cancer-carrying patients of Nagasaki atomic bomb survivors have multiple primary cancers in various tissues. This high-dose radiation exposure not only increased the risk of developing various types of cancer, but also worsened the overall survival (OS) rate. We recently reported significantly shorter OS among Nagasaki atomic bomb survivors with MDS versus patients without such radiation exposure (Jo et al., Anticancer Research 2015).
Aims
We investigated whether high-dose radiation exposure would similarly affect the incidence rates and outcomes of follicular lymphoma (FL) and diffuse large B-cell lymphoma (DLBCL).
Methods
The youngest atomic bomb survivors are aged approximately 70 years, presenting a challenge to perform prospective cohort studies. Therefore, we conducted a retrospective cohort study of the incidence rates and outcomes of FL and DLBCL in cases diagnosed at our hospital between January 2004 and December 2013. The primary objectives were to compare the incidence rates of FL and DLBCL in atomic bomb survivors (A-Bomb) and non-A-Bomb patients, and determine the OS rates.
Results
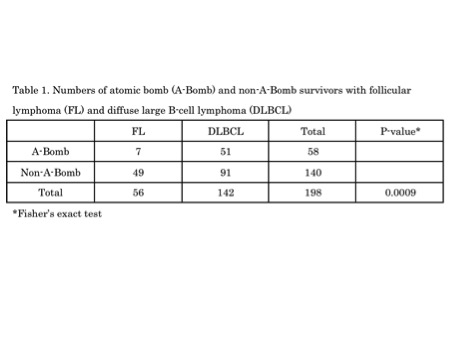
Table 1 lists the number of patients. Seven and 51 A-Bomb patients and 49 and 91 non-A-Bomb patients had FL and DLBCL, respectively. The incidence rate of FL versus DLBCL was significantly less among A-Bomb patients than among non-A-Bomb patients (P = 0.0009). There was no significant difference in OS between A-Bomb and non-A-Bomb patients with DLBCL (P = 0.3065, hazard ration [HR]: 1.311, 95% confidence interval [CI]: 0.7813–2.198). In contrast to DLBCL, the OS rate was significantly lower in A-Bomb patients with FL than in non-A-Bomb patients (P = 0.0092, HR: 5.425, 95% CI: 2.151–220.1). In both FL and DLBCL patients, there were no significant differences of background factors except for the median age between A-Bomb and non-A-Bomb patients. The respective median ages of A-Bomb and non-A-Bomb patients with DLBCL differed significantly at 75 (range, 62–91) and 73 (range, 17–93) years (P = 0.0038). The respective median ages of A-Bomb and non-A-Bomb patients with FL also differed significantly at 80 (range, 63–90) and 60 (range, 28–80) years (P < 0.0001). The age difference had no impact on the OS rate of DLBCL. Therefore, the shorter OS of A-Bomb patients with FL cannot be accounted only for the age difference between A-Bomb and non-A-Bomb patients. Some other unknown factors caused by high-dose radiation exposure of the Nagasaki Atomic Bomb could be linked to the OS difference.
Conclusion
Compared with non-A-Bomb patients, A-Bomb patients had a significantly lower FL incidence rate and significantly shorter OS. We previously reported significantly reduced OS among MDS patients exposed to the Nagasaki atomic bomb. These data suggest an influence of atomic bomb exposure and warrant further study for etiological clarification.
Session topic: E-poster
Keyword(s): Diffuse large B cell lymphoma, Follicular lymphoma, Radiation
{{ help_message }}
{{filter}}


