MOLECULAR AND CYTOGENETIC PROFILE OF PATIENTS WITH PRIMARY MYELOFIBROSIS
(Abstract release date: 05/19/16)
EHA Library. Poluskina L. 06/09/16; 134908; PB2008

Mrs. Liubov Poluskina
Contributions
Contributions
Abstract
Abstract: PB2008
Type: Publication Only
Background
Primary Myelofibrosis (PMF) is hematopoietic stem cell malignancy characterized by clonal proliferation of myeloid-lineage cells. The molecular basis of this event includes mutations in JAK2, MPL and CALR genes, called clonal markers (CM), cytogenetic abnormalities and epigenetic disorders. The variability of the clinical course among patients with PMF due to different CM and epigenetic status requires close analysis for possible stratification by risk groups.
Aims
The aim of our study was to estimate overall survival (OS) in PMF patients depending on the type of CM, cytogenetic and epigenetic features.
Methods
We have examined 89 patients with PMF. Median age was 59 years (range 19-82). For all patients the detection of V617F mutation of JAK2 was done. JAK2-negative samples were tested for MPL 515 codon mutations (PCR-RFLP) and 9th exon mutations of CALR gene by direct sequencing. Seventy-three patients underwent the analysis of mutations in EZH2 and ASXL1 genes with high resolution melting method followed by direct sequencing of probably mutated samples. Karyotype research was done for 39 patients with available bone marrow samples.
Results
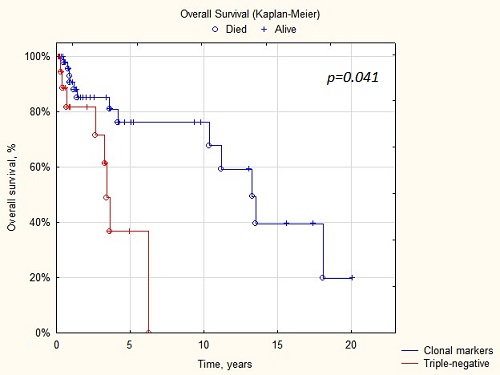
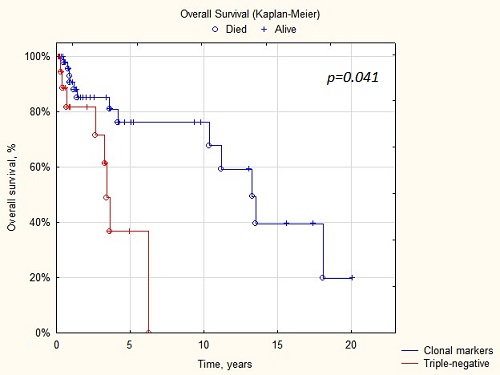
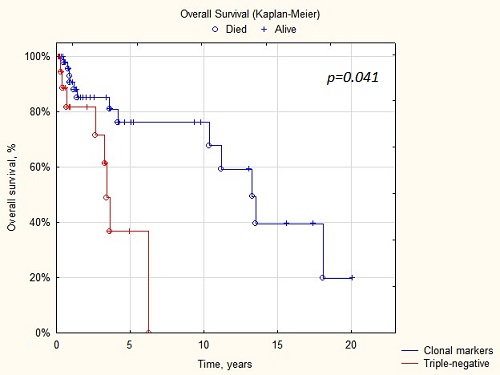
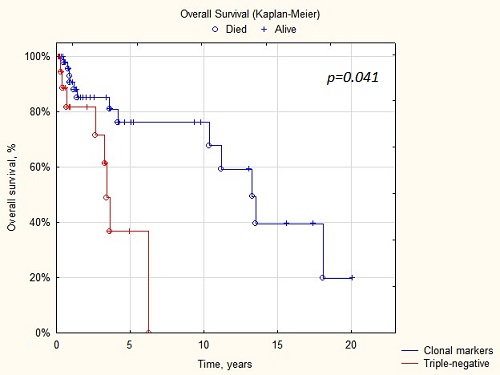
CM were detected in 64 patients: JAK2+ 46.1% (41/89), CALR+ 21.3% (19/89), MPL+ 4.5% (4/89) cases. No clonal markers were found in 28.1% (25/89) patients considered triple-negative (TN). Median survival of TN patients was the shortest and amounted to 4 years (p=0.041), JAK2+ 11.9 years. In CALR+ and MPL+ patients during follow-up of 10 and 4 years, respectively, median survival has not been reached.According to the results of cytogenetic analysis patients were divided into 2 groups: the first group included 20 patients with normal karyotype (NK) and 5 – with del(13)(q22), del(20)(q12), add(6)(p25), del(6)(q15) single features; the second group consisted of 13 patients with complex abnormalities and unfavorable aberrations (+8, -7/7q-, i(17q), inv(3), -5/5q-, 12p-). Median survival in the first group was 7.4 years, in the second group – 4.5 years. It should be noted separately that unfavorable karyotype frequency was distinct in groups with different CM: CALR+ 0% (0/8), JAK2+ 35% (6/17), TN 54% (7/13) cases (р=0.053).We have detected 18 mutations of ASXL1 gene in 16 patients (21.9%): fourteen patients had single mutation and two patients harbored 2 mutations at once. Mutation frequency was significantly higher in CALR+ patients compared to JAK2+ (37.5% (6/16) and 6.9% (2/29), р=0.037, resp.) and in TN patients compared to JAK2+ (33.3% (8/24) and 6.9% (2/29), р=0.044, resp.).Two mutations in EZH2 gene (2.2%) were observed in TN, ASXL1+ patients. Both cases characterized of high-risk progression of PMF. The first patient (men, 61-year-old, complex karyotype) progressed to blast phase rapidly from the diagnosis and died after 8 months. The second patient (men, 75-year-old, NK) had severe thrombocytopenia and died from hemorrhagic stroke after 5 months since the diagnosis.
Conclusion
Type of CM, cytogenetic aberrations and epigenetic changes can be correlated with different prognosis of PMF. The absence of CM and unfavorable karyotype are associated with reduced overall survival. The impact of epigenetic status on the prognosis in PMF patients requires further study.
Session topic: E-poster
Keyword(s): Molecular markers, Mutation, Myelofibrosis
Type: Publication Only
Background
Primary Myelofibrosis (PMF) is hematopoietic stem cell malignancy characterized by clonal proliferation of myeloid-lineage cells. The molecular basis of this event includes mutations in JAK2, MPL and CALR genes, called clonal markers (CM), cytogenetic abnormalities and epigenetic disorders. The variability of the clinical course among patients with PMF due to different CM and epigenetic status requires close analysis for possible stratification by risk groups.
Aims
The aim of our study was to estimate overall survival (OS) in PMF patients depending on the type of CM, cytogenetic and epigenetic features.
Methods
We have examined 89 patients with PMF. Median age was 59 years (range 19-82). For all patients the detection of V617F mutation of JAK2 was done. JAK2-negative samples were tested for MPL 515 codon mutations (PCR-RFLP) and 9th exon mutations of CALR gene by direct sequencing. Seventy-three patients underwent the analysis of mutations in EZH2 and ASXL1 genes with high resolution melting method followed by direct sequencing of probably mutated samples. Karyotype research was done for 39 patients with available bone marrow samples.
Results
CM were detected in 64 patients: JAK2+ 46.1% (41/89), CALR+ 21.3% (19/89), MPL+ 4.5% (4/89) cases. No clonal markers were found in 28.1% (25/89) patients considered triple-negative (TN). Median survival of TN patients was the shortest and amounted to 4 years (p=0.041), JAK2+ 11.9 years. In CALR+ and MPL+ patients during follow-up of 10 and 4 years, respectively, median survival has not been reached.According to the results of cytogenetic analysis patients were divided into 2 groups: the first group included 20 patients with normal karyotype (NK) and 5 – with del(13)(q22), del(20)(q12), add(6)(p25), del(6)(q15) single features; the second group consisted of 13 patients with complex abnormalities and unfavorable aberrations (+8, -7/7q-, i(17q), inv(3), -5/5q-, 12p-). Median survival in the first group was 7.4 years, in the second group – 4.5 years. It should be noted separately that unfavorable karyotype frequency was distinct in groups with different CM: CALR+ 0% (0/8), JAK2+ 35% (6/17), TN 54% (7/13) cases (р=0.053).We have detected 18 mutations of ASXL1 gene in 16 patients (21.9%): fourteen patients had single mutation and two patients harbored 2 mutations at once. Mutation frequency was significantly higher in CALR+ patients compared to JAK2+ (37.5% (6/16) and 6.9% (2/29), р=0.037, resp.) and in TN patients compared to JAK2+ (33.3% (8/24) and 6.9% (2/29), р=0.044, resp.).Two mutations in EZH2 gene (2.2%) were observed in TN, ASXL1+ patients. Both cases characterized of high-risk progression of PMF. The first patient (men, 61-year-old, complex karyotype) progressed to blast phase rapidly from the diagnosis and died after 8 months. The second patient (men, 75-year-old, NK) had severe thrombocytopenia and died from hemorrhagic stroke after 5 months since the diagnosis.
Conclusion
Type of CM, cytogenetic aberrations and epigenetic changes can be correlated with different prognosis of PMF. The absence of CM and unfavorable karyotype are associated with reduced overall survival. The impact of epigenetic status on the prognosis in PMF patients requires further study.
Session topic: E-poster
Keyword(s): Molecular markers, Mutation, Myelofibrosis
Abstract: PB2008
Type: Publication Only
Background
Primary Myelofibrosis (PMF) is hematopoietic stem cell malignancy characterized by clonal proliferation of myeloid-lineage cells. The molecular basis of this event includes mutations in JAK2, MPL and CALR genes, called clonal markers (CM), cytogenetic abnormalities and epigenetic disorders. The variability of the clinical course among patients with PMF due to different CM and epigenetic status requires close analysis for possible stratification by risk groups.
Aims
The aim of our study was to estimate overall survival (OS) in PMF patients depending on the type of CM, cytogenetic and epigenetic features.
Methods
We have examined 89 patients with PMF. Median age was 59 years (range 19-82). For all patients the detection of V617F mutation of JAK2 was done. JAK2-negative samples were tested for MPL 515 codon mutations (PCR-RFLP) and 9th exon mutations of CALR gene by direct sequencing. Seventy-three patients underwent the analysis of mutations in EZH2 and ASXL1 genes with high resolution melting method followed by direct sequencing of probably mutated samples. Karyotype research was done for 39 patients with available bone marrow samples.
Results
CM were detected in 64 patients: JAK2+ 46.1% (41/89), CALR+ 21.3% (19/89), MPL+ 4.5% (4/89) cases. No clonal markers were found in 28.1% (25/89) patients considered triple-negative (TN). Median survival of TN patients was the shortest and amounted to 4 years (p=0.041), JAK2+ 11.9 years. In CALR+ and MPL+ patients during follow-up of 10 and 4 years, respectively, median survival has not been reached.According to the results of cytogenetic analysis patients were divided into 2 groups: the first group included 20 patients with normal karyotype (NK) and 5 – with del(13)(q22), del(20)(q12), add(6)(p25), del(6)(q15) single features; the second group consisted of 13 patients with complex abnormalities and unfavorable aberrations (+8, -7/7q-, i(17q), inv(3), -5/5q-, 12p-). Median survival in the first group was 7.4 years, in the second group – 4.5 years. It should be noted separately that unfavorable karyotype frequency was distinct in groups with different CM: CALR+ 0% (0/8), JAK2+ 35% (6/17), TN 54% (7/13) cases (р=0.053).We have detected 18 mutations of ASXL1 gene in 16 patients (21.9%): fourteen patients had single mutation and two patients harbored 2 mutations at once. Mutation frequency was significantly higher in CALR+ patients compared to JAK2+ (37.5% (6/16) and 6.9% (2/29), р=0.037, resp.) and in TN patients compared to JAK2+ (33.3% (8/24) and 6.9% (2/29), р=0.044, resp.).Two mutations in EZH2 gene (2.2%) were observed in TN, ASXL1+ patients. Both cases characterized of high-risk progression of PMF. The first patient (men, 61-year-old, complex karyotype) progressed to blast phase rapidly from the diagnosis and died after 8 months. The second patient (men, 75-year-old, NK) had severe thrombocytopenia and died from hemorrhagic stroke after 5 months since the diagnosis.
Conclusion
Type of CM, cytogenetic aberrations and epigenetic changes can be correlated with different prognosis of PMF. The absence of CM and unfavorable karyotype are associated with reduced overall survival. The impact of epigenetic status on the prognosis in PMF patients requires further study.
Session topic: E-poster
Keyword(s): Molecular markers, Mutation, Myelofibrosis
Type: Publication Only
Background
Primary Myelofibrosis (PMF) is hematopoietic stem cell malignancy characterized by clonal proliferation of myeloid-lineage cells. The molecular basis of this event includes mutations in JAK2, MPL and CALR genes, called clonal markers (CM), cytogenetic abnormalities and epigenetic disorders. The variability of the clinical course among patients with PMF due to different CM and epigenetic status requires close analysis for possible stratification by risk groups.
Aims
The aim of our study was to estimate overall survival (OS) in PMF patients depending on the type of CM, cytogenetic and epigenetic features.
Methods
We have examined 89 patients with PMF. Median age was 59 years (range 19-82). For all patients the detection of V617F mutation of JAK2 was done. JAK2-negative samples were tested for MPL 515 codon mutations (PCR-RFLP) and 9th exon mutations of CALR gene by direct sequencing. Seventy-three patients underwent the analysis of mutations in EZH2 and ASXL1 genes with high resolution melting method followed by direct sequencing of probably mutated samples. Karyotype research was done for 39 patients with available bone marrow samples.
Results
CM were detected in 64 patients: JAK2+ 46.1% (41/89), CALR+ 21.3% (19/89), MPL+ 4.5% (4/89) cases. No clonal markers were found in 28.1% (25/89) patients considered triple-negative (TN). Median survival of TN patients was the shortest and amounted to 4 years (p=0.041), JAK2+ 11.9 years. In CALR+ and MPL+ patients during follow-up of 10 and 4 years, respectively, median survival has not been reached.According to the results of cytogenetic analysis patients were divided into 2 groups: the first group included 20 patients with normal karyotype (NK) and 5 – with del(13)(q22), del(20)(q12), add(6)(p25), del(6)(q15) single features; the second group consisted of 13 patients with complex abnormalities and unfavorable aberrations (+8, -7/7q-, i(17q), inv(3), -5/5q-, 12p-). Median survival in the first group was 7.4 years, in the second group – 4.5 years. It should be noted separately that unfavorable karyotype frequency was distinct in groups with different CM: CALR+ 0% (0/8), JAK2+ 35% (6/17), TN 54% (7/13) cases (р=0.053).We have detected 18 mutations of ASXL1 gene in 16 patients (21.9%): fourteen patients had single mutation and two patients harbored 2 mutations at once. Mutation frequency was significantly higher in CALR+ patients compared to JAK2+ (37.5% (6/16) and 6.9% (2/29), р=0.037, resp.) and in TN patients compared to JAK2+ (33.3% (8/24) and 6.9% (2/29), р=0.044, resp.).Two mutations in EZH2 gene (2.2%) were observed in TN, ASXL1+ patients. Both cases characterized of high-risk progression of PMF. The first patient (men, 61-year-old, complex karyotype) progressed to blast phase rapidly from the diagnosis and died after 8 months. The second patient (men, 75-year-old, NK) had severe thrombocytopenia and died from hemorrhagic stroke after 5 months since the diagnosis.
Conclusion
Type of CM, cytogenetic aberrations and epigenetic changes can be correlated with different prognosis of PMF. The absence of CM and unfavorable karyotype are associated with reduced overall survival. The impact of epigenetic status on the prognosis in PMF patients requires further study.
Session topic: E-poster
Keyword(s): Molecular markers, Mutation, Myelofibrosis
{{ help_message }}
{{filter}}


